Published online Jun 26, 2012. doi: 10.4330/wjc.v4.i6.218
Revised: June 6, 2012
Accepted: June 13, 2012
Published online: June 26, 2012
Left ventricular (LV) pseudoaneurysm is a late mechanical complication of myocardial infarction (MI). A giant LV pseudoaneurysm is a rare presentation. We report a case of a giant LV pseudoaneurysm in a post MI patient, who presented with hemoptysis. Hemoptysis is a rare clinical presentation of LV pseudoaneurysm. The patient had successful surgical repair of the aneurysm and had a favorable outcome in 9 mo’ follow-up. The imaging modalities and surgical treatment of a pseudoaneurysm is discussed.
- Citation: Vijayvergiya R, Pattam J, Rana SS, Singh JD, Puri GD, Singhal M. Giant left ventricular pseudoaneurysm presenting with hemoptysis. World J Cardiol 2012; 4(6): 218-220
- URL: https://www.wjgnet.com/1949-8462/full/v4/i6/218.htm
- DOI: https://dx.doi.org/10.4330/wjc.v4.i6.218
Left ventricular (LV) pseudoaneurysm is a contained cardiac rupture, which is sealed by layers of organized thrombus and hematoma. It is encircled by a thin layer of adherent pericardium without any myocardial layer, which makes it susceptible to rupture. The clinical presentation of pseudoaneurysm is variable. We hereby report an unusual case of giant LV pseudoaneurysm, presenting with recurrent hemoptysis and congestive cardiac failure. The role of various imaging modalities and surgical treatment of pseudoaneurysm is discussed.
A 60-year-old chronic smoking male presented in August 2009 with symptoms of chronic stable angina class 2 of 1 year duration, which worsened to class 3 in the preceding month. He had suffered an inferior wall myocardial infarction (MI) 3.5 years previously. His general physical examination was unremarkable. His cardiac examination revealed a LV 3rd heart sound, and chest examination revealed basal crepitations in both lung fields. An electrocardiogram showed T inversion in the inferior limb leads. An echocardiogram revealed global LV hypokinesia and an ejection fraction of 0.30. There was no mitral regurgitation. Coronary angiography revealed diffuse 70% mid right coronary artery (RCA) stenosis (Figure 1A). The left coronary artery and its branches were normal. He had successful percutaneous coronary intervention (PCI) of the mid RCA with a 2.75 mm × 33 mm bare metal stent (Presillion stent, Cordis Corp., Miami, Florida) (Figure 1B). Subsequently, he remained well on medical treatment.
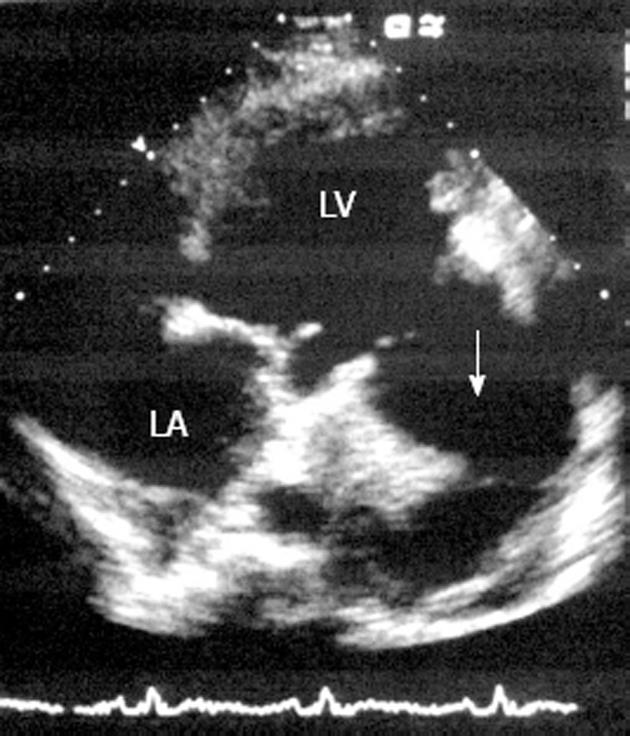
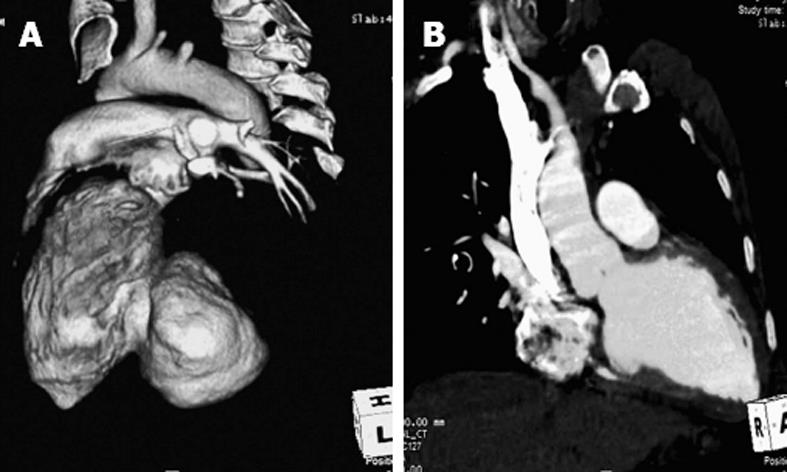
At 2 years’ follow-up in July 2011, he presented with recurrent hemoptysis of 1 wk duration. There was about 5-10 mL of blood in each bout of hemoptysis. A chest X-ray showed a cardio-thoracic ratio of 0.75; there was no radiological abnormality in either lung field. An echocardiogram showed a LV ejection fraction of 0.30 and no mitral regurgitation. There was a large LV pseudoaneurysm at the sub-mitral position, measuring 110 mm × 100 mm with a 44 mm neck. The pseudoaneurysm cavity was partially filled with a thrombus (Figure 2). A computed tomography (CT) scan of the chest showed a large contrast filled LV pseudoaneurysm arising from postero-lateral wall (Figure 3A), measuring 110 mm × 100 mm × 78 mm with a 42 mm neck. It was compressing the adjacent bronchus and lung parenchyma. The rest of the lung fields were normal. A small non-delineated communication of pseudoaneurysm with the lung parenchyma or bronchus was considered to be consistent with recurrent hemoptysis. A repeat cardiac catheterization revealed a patent RCA stent (Figure 1C) and normal left coronary artery system. A LV angiogram showed a large pseudoaneurysm arising from the lateral wall of the left ventricle.
The patient underwent surgical repair of the pseudoaneurysm. The left lateral wall of the heart was mobilized under cardio-pulmonary bypass. It was densely adherent to the pericardium and adjacent lingular segment of the left lung. Under cardioplegic arrest, the pseudoaneurysm was opened leaving a small rim of sac wall towards the lung. The pseudoaneurysm sac was filled with a blood clot (Figure 4A) and had a circular gap of about 40 mm diameter through which it was connected to the LV cavity (Figure 4B). The defect was closed using a polytetrafluoroethylene (PTFE) patch with interrupted 4-0 Prolene suture (Figure 4C). The false sac was tailored to make two flaps which firmly covered the PTFE patch. Biological glue was spread between the two layers before tying the last suture of the sac. The patient was weaned from cardiopulmonary bypass and had an uneventful postoperative recovery. A postoperative CT scan of the chest revealed normal LV outline without any leakage (Figure 3B). He was discharged on the 7th postoperative day. He remained asymptomatic at 9 mo’ follow-up with no recurrence of hemoptysis.
LV pseudoaneurysm is seen in patients having MI, cardiac infection, and following cardiac interventions or trauma[1]. MI is the most frequently observed etiology in LV pseudoaneurysm cases. It is a late mechanical complication of MI presenting within a few months of infarction. A very late presentation after years of MI as observed in the index case is very rare[2]. There was no evident pseudoaneurysm on echocardiographic evaluation at the time of PCI of the RCA, which was performed 3.5 years after MI. During subsequent follow-up following PCI, his heart failure symptoms were attributed to low ejection fraction of 0.30, though the LV pseudoaneurysm would have also contributed to it. In general, patients do not have specific symptoms pertaining to pseudoaneurysm[1], hence th timely diagnosis may be difficult. In the index case also, the pseudoaneurysm could have been diagnosed earlier if periodic echocardiography screening was performed following PCI. A giant LV pseudoaneurysm has been reported to cause mitral regurgitation and compression of the adjacent vascular structures[3-5]; however there were no such complications in the present case. Hemoptysis is a rare presentation of LV pseudoaneurysm[6]. It occurs following ventriculo-pulmonary communication and, if not diagnosed in time, carries a poor prognosis[6]. Due to our earlier experience of managing a case of intractable hemoptysis with LV pseudoaneurysm[6], we suspected pseudoaneurysm in this case also, and confirmed it by echocardiography and a subsequent CT scan. A high clinical suspicion and periodic echocardiographic screening can diagnose this entity in time for it to be properly managed. Both echocardiography and CT angiography are good noninvasive imaging modalities for pseudoaneurysm diagnosis[1,2,5,6]. A CT scan delineates the extent of a pseudoaneurysm, the involvement of adjacent cardiac and non-cardiac structures, and rules out other primary pulmonary causes of hemoptysis[6]. Surgery was indicated in the index case because of the symptomatic status, and the large size and impending rupture of the pseudoaneurysm, as manifested by recurrent hemoptysis. Surgery itself carries a high mortality[1]. Nevertheless we performed a successful PTFE patch repair of the pseudoaneurysm and the patient had an uneventful 9 mo of follow-up.
In conclusion, LV pseudoaneurysm can be a very late complication of MI. Hemoptysis is a rare presentation of LV pseudoaneurysm and indicates an impending rupture. A high clinical suspicion and periodic echocardiographic screening should be performed for early diagnosis and appropriate management of such cases.
Peer reviewer: Ricardo Castillo, MD, Cardiology, Brookdale University Hospital and Medical Center, One Brookdale plaza, Snapper building 3rd floor, Brooklyn, NY 11212, United States
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
| 1. | Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32:557-561. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 396] [Cited by in F6Publishing: 381] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 2. | Alizade E, Guler A, Acar G, Karakoyun S, Esen AM. Multimodality cardiac imaging of a giant left ventricular pseudoaneurysm. Eur J Echocardiogr. 2011;12:550. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 3. | Kansiz E, Hatemi AC, Tongut A, Cohcen S, Yildiz A, Kilickesmez K, Celiker C. Surgical treatment of a giant postero-inferior left ventricular pseudoaneurysm causing severe mitral insufficiency and congestive heart failure. Ann Thorac Cardiovasc Surg. 2012;18:151-155. [PubMed] [Cited in This Article: ] |
| 4. | Fox SA, Templeton C, Hancock-Friesen C, Chen R. Commotio cordis and ventricular pseudoaneurysm. Can J Cardiol. 2009;25:237-238. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Lee YH, Hou CJ, Hung CL, Tsai CH. Silent and huge left ventricular pseudoaneurysm with left atrial compression: dedicated spatial resolution and geometry by 3-dimensional echocardiography. J Am Soc Echocardiogr. 2007;20:772.e5-772.e9. [PubMed] [Cited in This Article: ] |
| 6. | Vijayvergiya R, Chongtham DS, Thingnam SK, Grover A, Lal A. Left ventricular pseudoaneurysm with infective pericarditis: a rare cause of intractable hemoptysis. Angiology. 2008;59:507-509. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |