-
PDF
- Split View
-
Views
-
Cite
Cite
Mercedes Medina-Ramón, Antonella Zanobetti, Joel Schwartz, The Effect of Ozone and PM10 on Hospital Admissions for Pneumonia and Chronic Obstructive Pulmonary Disease: A National Multicity Study, American Journal of Epidemiology, Volume 163, Issue 6, 15 March 2006, Pages 579–588, https://doi.org/10.1093/aje/kwj078
Close - Share Icon Share
Abstract
A case-crossover study was conducted in 36 US cities to evaluate the effect of ozone and particulate matter with an aerodynamic diameter of ≤10 μm (PM10) on respiratory hospital admissions and to identify which city characteristics may explain the heterogeneity in risk estimates. Respiratory hospital admissions and air pollution data were obtained for 1986–1999. In a meta-analysis based on the city-specific regression models, several city characteristics were evaluated as effect modifiers. During the warm season, the 2-day cumulative effect of a 5-ppb increase in ozone was a 0.27% (95% confidence interval (CI): 0.08, 0.47) increase in chronic obstructive pulmonary disease admissions and a 0.41% (95% CI: 0.26, 0.57) increase in pneumonia admissions. Similarly, a 10-μg/m3 increase in PM10 during the warm season resulted in a 1.47% (95% CI: 0.93, 2.01) increase in chronic obstructive pulmonary disease at lag 1 and a 0.84% (95% CI: 0.50, 1.19) increase in pneumonia at lag 0. Percentage of households with central air conditioning reduced the effect of air pollution, and variability of summer apparent temperature reduced the effect of ozone on chronic obstructive pulmonary disease. The study confirmed, in a large sample of cities, that exposure to ozone and PM10 is associated with respiratory hospital admissions and provided evidence that the effect of air pollution is modified by certain city characteristics.
Air pollution has been associated with hospital admissions for respiratory disease in cities all over the world (1–7). The most common and consistent associations have been found with particulate matter and tropospheric ozone (4). The magnitude of the effect of these pollutants, however, has differed substantially across locations. Moreover, many studies have examined all respiratory admissions, possibly combining outcomes with different sensitivities to air pollution and different lags between exposure and hospitalization. In addition, the number of cities examined in individual studies of respiratory admissions has generally been modest, particularly for ozone, and a large national sample would avoid selection bias, especially in light of evidence for heterogeneity in results across individual cities.
Because of limited numbers of locations, few studies have addressed the issue of whether the observed variability in exposure-effect relations can be explained by differences in meteorology, pollution sources, or socioeconomic characteristics of the cities. A study conducted in 14 US cities did not find evidence of modification by sociodemographic characteristics of the association between particulate matter with an aerodynamic diameter of ≤10 μm (PM10) and hospital admissions (8). A subsequent analysis using the same data found that the proportion of traffic-related particles in PM10 modified the effect of PM10 on hospital admissions for cardiovascular disease, but results were inconclusive for respiratory admissions (9). This study also found a stronger effect of PM10 on chronic obstructive pulmonary disease (COPD) admissions with decreasing proportion of central air conditioning, and similar results, although only marginally significant, were found for pneumonia admissions.
These studies had limited statistical power because they included a relatively small number of cities. In addition, they did not address modifiers of the association between ozone exposure and respiratory hospital admissions. We therefore conducted a large, multicity study in 36 US cities to evaluate the effect of daily PM10 and ozone concentrations on hospital admissions for COPD and for pneumonia and to assess whether the heterogeneity in the effect estimates across cities may be explained by differences in city characteristics such as meteorology, pollution sources, or socioeconomic factors.
MATERIALS AND METHODS
Study design
We conducted a case-crossover analysis using hospital admissions and air pollution data from 36 US cities during the period 1986–1999. We first selected cities that monitored PM10 daily and subsequently expanded the sample to include other large cities covering all regions of the United States. The cities selected were Albuquerque, New Mexico; Atlanta, Georgia; Baltimore, Maryland; Birmingham, Alabama; Boston, Massachusetts; Boulder, Colorado; Canton, Ohio; Chicago, Illinois; Cincinnati, Ohio; Cleveland, Ohio; Colorado Springs, Colorado; Columbus, Ohio; Denver, Colorado; Detroit, Michigan; Honolulu, Hawaii; Houston, Texas; Jersey City, New Jersey; Los Angeles, California; Minneapolis, Minnesota; Nashville, Tennessee; New Haven, Connecticut; New York City, New York; Palm Beach, Florida; Philadelphia, Pennsylvania; Pittsburgh, Pennsylvania; Provo, Utah; Sacramento, California; Salt Lake City, Utah; San Diego, California; San Francisco, California; Seattle, Washington; Steubenville, Ohio; St. Louis, Missouri; Spokane, Washington; Washington, DC; and Youngstown, Ohio.
The case-crossover design is a variant of the matched case-control design in which a case subject becomes a control subject on days when no event (hospital admission) occurs (10). By using control days close in time to the event day, there is no confounding by slowly varying personal characteristics since each subject is the perfect match for himself or herself. Bateson and Schwartz (11, 12) demonstrated that, by using such a matching scheme, even very strong seasonal confounding of exposure can be removed. If, in addition, as suggested by Levy et al. (13), we apply a time-stratified approach to choose the control days, a subtle selection bias can be avoided. A simulation study has shown that such an approach gives both unbiased estimates of effects and unbiased coverage probabilities (14). We followed this approach in our study by choosing control days only within the same month of the same year when the admission occurred (refer to the Statistical Analyses section of the text for more details on the specific selection criteria for days within that month).
Hospital admissions data
We extracted data on hospital admissions from the US Health Care Financing Administration (Medicare) billing records for the period 1986–1999. The Medicare system provides hospital coverage for all US citizens aged 65 years or older. The system includes data on type of admission, primary and secondary causes of admission, and other personal characteristics. Using this information, we selected for analyses those persons who had been admitted to the hospital on an emergency or urgent basis with a primary diagnosis of COPD (International Classification of Diseases, Ninth Revision: codes 490–496, except code 493) or pneumonia (International Classification of Diseases, Ninth Revision: codes 480–487).
Environmental data
We obtained air pollution data from the US Environmental Protection Agency's Aerometric Retrieval System (15). We estimated daily mean concentrations of ozone (8-hour) and PM10 (24-hour) for each city by using an algorithm that averaged levels reported by multiple monitoring locations (16). All cities except Minneapolis had daily measurements for ozone during the warm season (May–September), but only 16 had complete ozone measurements during the cold season (October–April). For all cities, PM10 levels were available throughout the year, although frequency of measurements varied across cities and within a city, with measurements typically made every 2, 3, or 6 days.
For each city, we obtained daily mean temperature and relative humidity from the nearest National Weather Service surface station (EarthInfo Inc., Boulder, Colorado). We used this information to calculate the apparent temperature, a composite index of perceived air temperature at a given humidity, previously used to control for weather in air pollution studies (17–20).
City characteristics
For each city, we calculated the mean and variance of the daily summer (June–August) apparent temperature by using the data described above. We calculated the percentage of people aged 65 years or older living in poverty by using data from the 1990 US Census. We calculated the percentage of households with central air conditioning by using data from the American Housing Survey of the US Census Bureau (21) for the period 1994–2002. We calculated the average annual mortality rate for emphysema among people aged 65 years or older by using data from the National Center for Health Statistics during 1989–2000. We took the latter as an indication of the smoking history of the population. Finally, we calculated the percentage of ambient PM10 from traffic (highway vehicles) by using data from the National Emission Trends 1996 (NET96) of the Environmental Protection Agency (22).
Statistical analyses
In the first stage of the analyses, we analyzed the association between exposure to air pollution and hospital admissions (for COPD and for pneumonia) by using city-specific conditional logistic regression models (the PROC PHREG procedure in SAS version 8.2 software, 2001; SAS Institute, Inc., Cary, North Carolina). We fitted separate models for ozone and PM10 exposure. For each hospitalization, we selected control days within the same month of the same year, leaving at least 2 days between each control day to minimize serial correlation. In all analyses, we controlled for day of the week and weather—the latter by using one cubic regression spline for the same day's apparent temperature and another for the previous day's apparent temperature.
For the ozone analysis, we examined the effect of exposure on the same day (lag 0) and on the day before (lag 1) admission. For each city, we first fitted a model including lag 0 and lag 1, then calculated the cumulative risk estimate for ozone exposure by summing the estimates from lag 0 and lag 1. We computed the overall standard error (SE) of the cumulative estimate as SE = sqrt[var(lag 0) + var(lag 1) + 2 × cov(lag 0, lag 1)].
Because PM10 was predominantly measured during nonconsecutive days, we assessed the effect of exposure to PM10 at lag 0 and lag 1 in separate models. We repeated the analyses of ozone and PM10 by examining separate effects for exposure in the warm season and in the cold season.
As a sensitivity analysis, we tested the use of an alternative matching scheme by selecting control days within the same month of the same year of the event and matching on apparent temperature (same rounded degrees Centigrade). In this analysis, we included in all models a cubic spline for the previous day's apparent temperature and indicator variables for day of the week. These models, by matching on temperature and month, control for potentially nonlinear temperature effects and for any interaction between temperature and month of the year (18). To study the effect of ozone exposure, we additionally tested a matching scheme that selected control days within the same month of the same year of the event and matched on day of the week. In this instance, models included a cubic spline for apparent temperature on the same day and another cubic spline for the previous day's apparent temperature. Because of the irregular sampling scheme for PM10, we could not follow this approach for PM10.
In the second stage of the analyses, we combined the city-specific results in a meta-analysis by using restricted maximum likelihood random-effects models (REML in Stata version 8 software; Stata Corporation, College Station, Texas) (23). After estimating the overall effect of ozone and PM10 on hospital admissions, we assessed the potential for effect modification of several city characteristics by including them (one at a time) as covariates in the meta-regression models. Then, we used the estimated model coefficients to predict the effect of air pollution on hospital admissions at the 25th and the 75th percentiles of the distribution of each city characteristic. A significant difference between these two predicted values indicates that the city characteristic modifies the effect of air pollution on hospital admissions, that is, the existence of an interaction between air pollution and the city characteristic.
RESULTS
Our analyses included 578,006 COPD admissions and 1,384,813 pneumonia admissions. Table 1 shows the counts of hospital admissions and describes the main environmental variables for each city. Ozone levels were higher in the warm season (average across all cities, 45.8 ppb (standard deviation, 9.2)) than in the cold season (27.6 ppb (standard deviation, 6.3)). PM10 levels were similar during both seasons, with an average concentration across all cities of 30.4 μg/m3 (standard deviation, 5.1). Los Angeles had the highest average levels of both ozone and PM10.
Environmental variables and respiratory hospital admissions in 36 US cities during 1986–1999
City, state . | Mean (SD*) ozone level (ppb) . | . | Mean (SD) PM10* level (μg/m3) . | Mean (SD) apparent temperature (°C) . | Total population aged ≥65 years (no.) . | COPD* admissions (no.) . | Pneumonia admissions (no.) . | |
|---|---|---|---|---|---|---|---|---|
| . | Warm season . | Cold season . | . | . | . | . | . | |
| Albuquerque, New Mexico | 50.5 (9.3) | 34.5 (10.2) | 27.9 (16.5) | 12.2 (8.9) | 50,379 | 3,115 | 9,035 | |
| Atlanta, Georgia | 55.9 (21.4) | 33.0 (16.4) | 17.1 (10.2) | 155,955 | 15,503 | 36,488 | ||
| Baltimore, Maryland | 52.3 (20.2) | 26.8 (13.0) | 32.4 (17.1) | 13.0 (11.1) | 197,438 | 19,950 | 40,858 | |
| Birmingham, Alabama | 49.7 (17.0) | 36.1 (21.0) | 17.4 (10.5) | 119,809 | 13,134 | 33,011 | ||
| Boston, Massachusetts | 42.3 (17.8) | 28.3 (11.3) | 25.4 (11.7) | 10.0 (10.3) | 342,322 | 34,700 | 88,936 | |
| Boulder, Colorado | 51.3 (14.2) | 24.2 (15.5) | 8.5 (9.7) | 17,048 | 1,678 | 3,427 | ||
| Canton, Ohio | 52.6 (17.8) | 26.1 (12.6) | 9.3 (11.2) | 53,216 | 7,534 | 12,965 | ||
| Chicago, Illinois | 40.0 (16.1) | 22.7 (9.8) | 33.6 (17.4) | 9.5 (11.9) | 631,826 | 49,581 | 142,576 | |
| Cincinnati, Ohio | 50.0 (17.8) | 32.2 (15.6) | 11.9 (11.5) | 115,000 | 10,797 | 33,323 | ||
| Cleveland, Ohio | 44.6 (17.6) | 37.1 (19.1) | 9.8 (11.3) | 220,659 | 29,947 | 50,262 | ||
| Colorado Springs, Colorado | 45.5 (11.3) | 30.4 (11.6) | 23.3 (13.4) | 7.8 (9.0) | 31,674 | 2,497 | 5,729 | |
| Columbus, Ohio | 49.8 (18.1) | 30.5 (14.6) | 11.1 (11.5) | 92,485 | 12,571 | 21,900 | ||
| Denver, Colorado | 44.0 (14.0) | 22.1 (12.7) | 33.2 (18.8) | 8.5 (9.7) | 64,152 | 4,219 | 11,820 | |
| Detroit, Michigan | 41.7 (17.2) | 33.7 (19.7) | 9.3 (11.5) | 263,997 | 5,751 | 12,393 | ||
| Honolulu, Hawaii | 15.0 (8.4) | 15.9 (6.2) | 27.5 (2.9) | 91,485 | 28,404 | 57,682 | ||
| Houston, Texas | 44.9 (22.1) | 32.9 (17.1) | 30.3 (16.0) | 22.2 (10.1) | 196,474 | 3,798 | 14,463 | |
| Jersey City, New Jersey | 50.3 (23.4) | 32.2 (17.0) | 12.4 (11.1) | 70,014 | 18,863 | 41,754 | ||
| Los Angeles, California | 63.0 (23.4) | 31.4 (20.2) | 44.0 (19.3) | 16.5 (4.3) | 855,666 | 9,211 | 12,645 | |
| Minneapolis, Minnesota | 27.3 (14.6) | 7.4 (12.5) | 175,854 | 63,316 | 174,241 | |||
| Nashville, Tennessee | 44.9 (16.8) | 23.9 (13.5) | 32.2 (14.9) | 15.5 (11.3) | 59,235 | 9,805 | 26,923 | |
| New Haven, Connecticut | 45.4 (19.5) | 26.0 (16.1) | 9.6 (10.8) | 117,863 | 5,962 | 14,719 | ||
| New York City, New York | 41.0 (19.5) | 19.7 (10.0) | 28.9 (13.9) | 12.5 (10.8) | 952,731 | 8,082 | 22,954 | |
| Palm Beach, Florida | 28.6 (12.7) | 33.7 (12.0) | 20.0 (8.1) | 27.1 (6.3) | 210,389 | 70,181 | 187,043 | |
| Philadelphia, Pennsylvania | 47.8 (21.0) | 23.0 (13.0) | 32.1 (15.8) | 12.9 (11.1) | 241,206 | 10,626 | 22,170 | |
| Pittsburgh, Pennsylvania | 48.4 (19.9) | 30.3 (20.0) | 10.3 (10.9) | 232,505 | 26,604 | 47,126 | ||
| Provo, Utah | 54.6 (10.9) | 35.1 (26.7) | 9.6 (10.4) | 18,429 | 33,408 | 52,148 | ||
| Sacramento, California | 55.6 (15.7) | 32.7 (14.2) | 31.1 (19.7) | 14.4 (7.0) | 109,674 | 718 | 4,081 | |
| Salt Lake City, Utah | 54.0 (12.5) | 35.7 (23.9) | 9.6 (10.4) | 61,079 | 8,680 | 21,840 | ||
| San Diego, California | 47.6 (12.1) | 40.4 (15.2) | 33.3 (13.1) | 17.0 (4.4) | 272,348 | 2,090 | 9,348 | |
| San Francisco, California | 22.8 (8.1) | 19.3 (10.2) | 27.7 (16.8) | 12.6 (3.8) | 105,263 | 17,632 | 43,446 | |
| Seattle, Washington | 35.0 (14.2) | 28.8 (18.6) | 9.5 (6.3) | 167,328 | 4,711 | 18,139 | ||
| Steubenville, Ohio | 46.1 (17.3) | 34.7 (19.9) | 10.3 (10.9) | 23,878 | 9,334 | 23,732 | ||
| St. Louis, Missouri | 48.4 (17.1) | 27.7 (12.7) | 13.7 (12.3) | 214,492 | 4,039 | 9,412 | ||
| Spokane, Washington | 44.6 (10.4) | 32.2 (28.3) | 6.5 (9.0) | 47,877 | 5,633 | 8,976 | ||
| Washington, DC | 48.4 (20.2) | 20.1 (12.3) | 27.7 (13.4) | 14.2 (11.2) | 77,672 | 17,665 | 54,386 | |
| Youngstown, Ohio | 47.1 (20.3) | 31.2 (15.6) | 8.9 (11.0) | 61,122 | 8,267 | 14,862 | ||
City, state . | Mean (SD*) ozone level (ppb) . | . | Mean (SD) PM10* level (μg/m3) . | Mean (SD) apparent temperature (°C) . | Total population aged ≥65 years (no.) . | COPD* admissions (no.) . | Pneumonia admissions (no.) . | |
|---|---|---|---|---|---|---|---|---|
| . | Warm season . | Cold season . | . | . | . | . | . | |
| Albuquerque, New Mexico | 50.5 (9.3) | 34.5 (10.2) | 27.9 (16.5) | 12.2 (8.9) | 50,379 | 3,115 | 9,035 | |
| Atlanta, Georgia | 55.9 (21.4) | 33.0 (16.4) | 17.1 (10.2) | 155,955 | 15,503 | 36,488 | ||
| Baltimore, Maryland | 52.3 (20.2) | 26.8 (13.0) | 32.4 (17.1) | 13.0 (11.1) | 197,438 | 19,950 | 40,858 | |
| Birmingham, Alabama | 49.7 (17.0) | 36.1 (21.0) | 17.4 (10.5) | 119,809 | 13,134 | 33,011 | ||
| Boston, Massachusetts | 42.3 (17.8) | 28.3 (11.3) | 25.4 (11.7) | 10.0 (10.3) | 342,322 | 34,700 | 88,936 | |
| Boulder, Colorado | 51.3 (14.2) | 24.2 (15.5) | 8.5 (9.7) | 17,048 | 1,678 | 3,427 | ||
| Canton, Ohio | 52.6 (17.8) | 26.1 (12.6) | 9.3 (11.2) | 53,216 | 7,534 | 12,965 | ||
| Chicago, Illinois | 40.0 (16.1) | 22.7 (9.8) | 33.6 (17.4) | 9.5 (11.9) | 631,826 | 49,581 | 142,576 | |
| Cincinnati, Ohio | 50.0 (17.8) | 32.2 (15.6) | 11.9 (11.5) | 115,000 | 10,797 | 33,323 | ||
| Cleveland, Ohio | 44.6 (17.6) | 37.1 (19.1) | 9.8 (11.3) | 220,659 | 29,947 | 50,262 | ||
| Colorado Springs, Colorado | 45.5 (11.3) | 30.4 (11.6) | 23.3 (13.4) | 7.8 (9.0) | 31,674 | 2,497 | 5,729 | |
| Columbus, Ohio | 49.8 (18.1) | 30.5 (14.6) | 11.1 (11.5) | 92,485 | 12,571 | 21,900 | ||
| Denver, Colorado | 44.0 (14.0) | 22.1 (12.7) | 33.2 (18.8) | 8.5 (9.7) | 64,152 | 4,219 | 11,820 | |
| Detroit, Michigan | 41.7 (17.2) | 33.7 (19.7) | 9.3 (11.5) | 263,997 | 5,751 | 12,393 | ||
| Honolulu, Hawaii | 15.0 (8.4) | 15.9 (6.2) | 27.5 (2.9) | 91,485 | 28,404 | 57,682 | ||
| Houston, Texas | 44.9 (22.1) | 32.9 (17.1) | 30.3 (16.0) | 22.2 (10.1) | 196,474 | 3,798 | 14,463 | |
| Jersey City, New Jersey | 50.3 (23.4) | 32.2 (17.0) | 12.4 (11.1) | 70,014 | 18,863 | 41,754 | ||
| Los Angeles, California | 63.0 (23.4) | 31.4 (20.2) | 44.0 (19.3) | 16.5 (4.3) | 855,666 | 9,211 | 12,645 | |
| Minneapolis, Minnesota | 27.3 (14.6) | 7.4 (12.5) | 175,854 | 63,316 | 174,241 | |||
| Nashville, Tennessee | 44.9 (16.8) | 23.9 (13.5) | 32.2 (14.9) | 15.5 (11.3) | 59,235 | 9,805 | 26,923 | |
| New Haven, Connecticut | 45.4 (19.5) | 26.0 (16.1) | 9.6 (10.8) | 117,863 | 5,962 | 14,719 | ||
| New York City, New York | 41.0 (19.5) | 19.7 (10.0) | 28.9 (13.9) | 12.5 (10.8) | 952,731 | 8,082 | 22,954 | |
| Palm Beach, Florida | 28.6 (12.7) | 33.7 (12.0) | 20.0 (8.1) | 27.1 (6.3) | 210,389 | 70,181 | 187,043 | |
| Philadelphia, Pennsylvania | 47.8 (21.0) | 23.0 (13.0) | 32.1 (15.8) | 12.9 (11.1) | 241,206 | 10,626 | 22,170 | |
| Pittsburgh, Pennsylvania | 48.4 (19.9) | 30.3 (20.0) | 10.3 (10.9) | 232,505 | 26,604 | 47,126 | ||
| Provo, Utah | 54.6 (10.9) | 35.1 (26.7) | 9.6 (10.4) | 18,429 | 33,408 | 52,148 | ||
| Sacramento, California | 55.6 (15.7) | 32.7 (14.2) | 31.1 (19.7) | 14.4 (7.0) | 109,674 | 718 | 4,081 | |
| Salt Lake City, Utah | 54.0 (12.5) | 35.7 (23.9) | 9.6 (10.4) | 61,079 | 8,680 | 21,840 | ||
| San Diego, California | 47.6 (12.1) | 40.4 (15.2) | 33.3 (13.1) | 17.0 (4.4) | 272,348 | 2,090 | 9,348 | |
| San Francisco, California | 22.8 (8.1) | 19.3 (10.2) | 27.7 (16.8) | 12.6 (3.8) | 105,263 | 17,632 | 43,446 | |
| Seattle, Washington | 35.0 (14.2) | 28.8 (18.6) | 9.5 (6.3) | 167,328 | 4,711 | 18,139 | ||
| Steubenville, Ohio | 46.1 (17.3) | 34.7 (19.9) | 10.3 (10.9) | 23,878 | 9,334 | 23,732 | ||
| St. Louis, Missouri | 48.4 (17.1) | 27.7 (12.7) | 13.7 (12.3) | 214,492 | 4,039 | 9,412 | ||
| Spokane, Washington | 44.6 (10.4) | 32.2 (28.3) | 6.5 (9.0) | 47,877 | 5,633 | 8,976 | ||
| Washington, DC | 48.4 (20.2) | 20.1 (12.3) | 27.7 (13.4) | 14.2 (11.2) | 77,672 | 17,665 | 54,386 | |
| Youngstown, Ohio | 47.1 (20.3) | 31.2 (15.6) | 8.9 (11.0) | 61,122 | 8,267 | 14,862 | ||
SD, standard deviation; PM10, particulate matter with an aerodynamic diameter of ≤10 μm; COPD, chronic obstructive pulmonary disease.
Environmental variables and respiratory hospital admissions in 36 US cities during 1986–1999
City, state . | Mean (SD*) ozone level (ppb) . | . | Mean (SD) PM10* level (μg/m3) . | Mean (SD) apparent temperature (°C) . | Total population aged ≥65 years (no.) . | COPD* admissions (no.) . | Pneumonia admissions (no.) . | |
|---|---|---|---|---|---|---|---|---|
| . | Warm season . | Cold season . | . | . | . | . | . | |
| Albuquerque, New Mexico | 50.5 (9.3) | 34.5 (10.2) | 27.9 (16.5) | 12.2 (8.9) | 50,379 | 3,115 | 9,035 | |
| Atlanta, Georgia | 55.9 (21.4) | 33.0 (16.4) | 17.1 (10.2) | 155,955 | 15,503 | 36,488 | ||
| Baltimore, Maryland | 52.3 (20.2) | 26.8 (13.0) | 32.4 (17.1) | 13.0 (11.1) | 197,438 | 19,950 | 40,858 | |
| Birmingham, Alabama | 49.7 (17.0) | 36.1 (21.0) | 17.4 (10.5) | 119,809 | 13,134 | 33,011 | ||
| Boston, Massachusetts | 42.3 (17.8) | 28.3 (11.3) | 25.4 (11.7) | 10.0 (10.3) | 342,322 | 34,700 | 88,936 | |
| Boulder, Colorado | 51.3 (14.2) | 24.2 (15.5) | 8.5 (9.7) | 17,048 | 1,678 | 3,427 | ||
| Canton, Ohio | 52.6 (17.8) | 26.1 (12.6) | 9.3 (11.2) | 53,216 | 7,534 | 12,965 | ||
| Chicago, Illinois | 40.0 (16.1) | 22.7 (9.8) | 33.6 (17.4) | 9.5 (11.9) | 631,826 | 49,581 | 142,576 | |
| Cincinnati, Ohio | 50.0 (17.8) | 32.2 (15.6) | 11.9 (11.5) | 115,000 | 10,797 | 33,323 | ||
| Cleveland, Ohio | 44.6 (17.6) | 37.1 (19.1) | 9.8 (11.3) | 220,659 | 29,947 | 50,262 | ||
| Colorado Springs, Colorado | 45.5 (11.3) | 30.4 (11.6) | 23.3 (13.4) | 7.8 (9.0) | 31,674 | 2,497 | 5,729 | |
| Columbus, Ohio | 49.8 (18.1) | 30.5 (14.6) | 11.1 (11.5) | 92,485 | 12,571 | 21,900 | ||
| Denver, Colorado | 44.0 (14.0) | 22.1 (12.7) | 33.2 (18.8) | 8.5 (9.7) | 64,152 | 4,219 | 11,820 | |
| Detroit, Michigan | 41.7 (17.2) | 33.7 (19.7) | 9.3 (11.5) | 263,997 | 5,751 | 12,393 | ||
| Honolulu, Hawaii | 15.0 (8.4) | 15.9 (6.2) | 27.5 (2.9) | 91,485 | 28,404 | 57,682 | ||
| Houston, Texas | 44.9 (22.1) | 32.9 (17.1) | 30.3 (16.0) | 22.2 (10.1) | 196,474 | 3,798 | 14,463 | |
| Jersey City, New Jersey | 50.3 (23.4) | 32.2 (17.0) | 12.4 (11.1) | 70,014 | 18,863 | 41,754 | ||
| Los Angeles, California | 63.0 (23.4) | 31.4 (20.2) | 44.0 (19.3) | 16.5 (4.3) | 855,666 | 9,211 | 12,645 | |
| Minneapolis, Minnesota | 27.3 (14.6) | 7.4 (12.5) | 175,854 | 63,316 | 174,241 | |||
| Nashville, Tennessee | 44.9 (16.8) | 23.9 (13.5) | 32.2 (14.9) | 15.5 (11.3) | 59,235 | 9,805 | 26,923 | |
| New Haven, Connecticut | 45.4 (19.5) | 26.0 (16.1) | 9.6 (10.8) | 117,863 | 5,962 | 14,719 | ||
| New York City, New York | 41.0 (19.5) | 19.7 (10.0) | 28.9 (13.9) | 12.5 (10.8) | 952,731 | 8,082 | 22,954 | |
| Palm Beach, Florida | 28.6 (12.7) | 33.7 (12.0) | 20.0 (8.1) | 27.1 (6.3) | 210,389 | 70,181 | 187,043 | |
| Philadelphia, Pennsylvania | 47.8 (21.0) | 23.0 (13.0) | 32.1 (15.8) | 12.9 (11.1) | 241,206 | 10,626 | 22,170 | |
| Pittsburgh, Pennsylvania | 48.4 (19.9) | 30.3 (20.0) | 10.3 (10.9) | 232,505 | 26,604 | 47,126 | ||
| Provo, Utah | 54.6 (10.9) | 35.1 (26.7) | 9.6 (10.4) | 18,429 | 33,408 | 52,148 | ||
| Sacramento, California | 55.6 (15.7) | 32.7 (14.2) | 31.1 (19.7) | 14.4 (7.0) | 109,674 | 718 | 4,081 | |
| Salt Lake City, Utah | 54.0 (12.5) | 35.7 (23.9) | 9.6 (10.4) | 61,079 | 8,680 | 21,840 | ||
| San Diego, California | 47.6 (12.1) | 40.4 (15.2) | 33.3 (13.1) | 17.0 (4.4) | 272,348 | 2,090 | 9,348 | |
| San Francisco, California | 22.8 (8.1) | 19.3 (10.2) | 27.7 (16.8) | 12.6 (3.8) | 105,263 | 17,632 | 43,446 | |
| Seattle, Washington | 35.0 (14.2) | 28.8 (18.6) | 9.5 (6.3) | 167,328 | 4,711 | 18,139 | ||
| Steubenville, Ohio | 46.1 (17.3) | 34.7 (19.9) | 10.3 (10.9) | 23,878 | 9,334 | 23,732 | ||
| St. Louis, Missouri | 48.4 (17.1) | 27.7 (12.7) | 13.7 (12.3) | 214,492 | 4,039 | 9,412 | ||
| Spokane, Washington | 44.6 (10.4) | 32.2 (28.3) | 6.5 (9.0) | 47,877 | 5,633 | 8,976 | ||
| Washington, DC | 48.4 (20.2) | 20.1 (12.3) | 27.7 (13.4) | 14.2 (11.2) | 77,672 | 17,665 | 54,386 | |
| Youngstown, Ohio | 47.1 (20.3) | 31.2 (15.6) | 8.9 (11.0) | 61,122 | 8,267 | 14,862 | ||
City, state . | Mean (SD*) ozone level (ppb) . | . | Mean (SD) PM10* level (μg/m3) . | Mean (SD) apparent temperature (°C) . | Total population aged ≥65 years (no.) . | COPD* admissions (no.) . | Pneumonia admissions (no.) . | |
|---|---|---|---|---|---|---|---|---|
| . | Warm season . | Cold season . | . | . | . | . | . | |
| Albuquerque, New Mexico | 50.5 (9.3) | 34.5 (10.2) | 27.9 (16.5) | 12.2 (8.9) | 50,379 | 3,115 | 9,035 | |
| Atlanta, Georgia | 55.9 (21.4) | 33.0 (16.4) | 17.1 (10.2) | 155,955 | 15,503 | 36,488 | ||
| Baltimore, Maryland | 52.3 (20.2) | 26.8 (13.0) | 32.4 (17.1) | 13.0 (11.1) | 197,438 | 19,950 | 40,858 | |
| Birmingham, Alabama | 49.7 (17.0) | 36.1 (21.0) | 17.4 (10.5) | 119,809 | 13,134 | 33,011 | ||
| Boston, Massachusetts | 42.3 (17.8) | 28.3 (11.3) | 25.4 (11.7) | 10.0 (10.3) | 342,322 | 34,700 | 88,936 | |
| Boulder, Colorado | 51.3 (14.2) | 24.2 (15.5) | 8.5 (9.7) | 17,048 | 1,678 | 3,427 | ||
| Canton, Ohio | 52.6 (17.8) | 26.1 (12.6) | 9.3 (11.2) | 53,216 | 7,534 | 12,965 | ||
| Chicago, Illinois | 40.0 (16.1) | 22.7 (9.8) | 33.6 (17.4) | 9.5 (11.9) | 631,826 | 49,581 | 142,576 | |
| Cincinnati, Ohio | 50.0 (17.8) | 32.2 (15.6) | 11.9 (11.5) | 115,000 | 10,797 | 33,323 | ||
| Cleveland, Ohio | 44.6 (17.6) | 37.1 (19.1) | 9.8 (11.3) | 220,659 | 29,947 | 50,262 | ||
| Colorado Springs, Colorado | 45.5 (11.3) | 30.4 (11.6) | 23.3 (13.4) | 7.8 (9.0) | 31,674 | 2,497 | 5,729 | |
| Columbus, Ohio | 49.8 (18.1) | 30.5 (14.6) | 11.1 (11.5) | 92,485 | 12,571 | 21,900 | ||
| Denver, Colorado | 44.0 (14.0) | 22.1 (12.7) | 33.2 (18.8) | 8.5 (9.7) | 64,152 | 4,219 | 11,820 | |
| Detroit, Michigan | 41.7 (17.2) | 33.7 (19.7) | 9.3 (11.5) | 263,997 | 5,751 | 12,393 | ||
| Honolulu, Hawaii | 15.0 (8.4) | 15.9 (6.2) | 27.5 (2.9) | 91,485 | 28,404 | 57,682 | ||
| Houston, Texas | 44.9 (22.1) | 32.9 (17.1) | 30.3 (16.0) | 22.2 (10.1) | 196,474 | 3,798 | 14,463 | |
| Jersey City, New Jersey | 50.3 (23.4) | 32.2 (17.0) | 12.4 (11.1) | 70,014 | 18,863 | 41,754 | ||
| Los Angeles, California | 63.0 (23.4) | 31.4 (20.2) | 44.0 (19.3) | 16.5 (4.3) | 855,666 | 9,211 | 12,645 | |
| Minneapolis, Minnesota | 27.3 (14.6) | 7.4 (12.5) | 175,854 | 63,316 | 174,241 | |||
| Nashville, Tennessee | 44.9 (16.8) | 23.9 (13.5) | 32.2 (14.9) | 15.5 (11.3) | 59,235 | 9,805 | 26,923 | |
| New Haven, Connecticut | 45.4 (19.5) | 26.0 (16.1) | 9.6 (10.8) | 117,863 | 5,962 | 14,719 | ||
| New York City, New York | 41.0 (19.5) | 19.7 (10.0) | 28.9 (13.9) | 12.5 (10.8) | 952,731 | 8,082 | 22,954 | |
| Palm Beach, Florida | 28.6 (12.7) | 33.7 (12.0) | 20.0 (8.1) | 27.1 (6.3) | 210,389 | 70,181 | 187,043 | |
| Philadelphia, Pennsylvania | 47.8 (21.0) | 23.0 (13.0) | 32.1 (15.8) | 12.9 (11.1) | 241,206 | 10,626 | 22,170 | |
| Pittsburgh, Pennsylvania | 48.4 (19.9) | 30.3 (20.0) | 10.3 (10.9) | 232,505 | 26,604 | 47,126 | ||
| Provo, Utah | 54.6 (10.9) | 35.1 (26.7) | 9.6 (10.4) | 18,429 | 33,408 | 52,148 | ||
| Sacramento, California | 55.6 (15.7) | 32.7 (14.2) | 31.1 (19.7) | 14.4 (7.0) | 109,674 | 718 | 4,081 | |
| Salt Lake City, Utah | 54.0 (12.5) | 35.7 (23.9) | 9.6 (10.4) | 61,079 | 8,680 | 21,840 | ||
| San Diego, California | 47.6 (12.1) | 40.4 (15.2) | 33.3 (13.1) | 17.0 (4.4) | 272,348 | 2,090 | 9,348 | |
| San Francisco, California | 22.8 (8.1) | 19.3 (10.2) | 27.7 (16.8) | 12.6 (3.8) | 105,263 | 17,632 | 43,446 | |
| Seattle, Washington | 35.0 (14.2) | 28.8 (18.6) | 9.5 (6.3) | 167,328 | 4,711 | 18,139 | ||
| Steubenville, Ohio | 46.1 (17.3) | 34.7 (19.9) | 10.3 (10.9) | 23,878 | 9,334 | 23,732 | ||
| St. Louis, Missouri | 48.4 (17.1) | 27.7 (12.7) | 13.7 (12.3) | 214,492 | 4,039 | 9,412 | ||
| Spokane, Washington | 44.6 (10.4) | 32.2 (28.3) | 6.5 (9.0) | 47,877 | 5,633 | 8,976 | ||
| Washington, DC | 48.4 (20.2) | 20.1 (12.3) | 27.7 (13.4) | 14.2 (11.2) | 77,672 | 17,665 | 54,386 | |
| Youngstown, Ohio | 47.1 (20.3) | 31.2 (15.6) | 8.9 (11.0) | 61,122 | 8,267 | 14,862 | ||
SD, standard deviation; PM10, particulate matter with an aerodynamic diameter of ≤10 μm; COPD, chronic obstructive pulmonary disease.
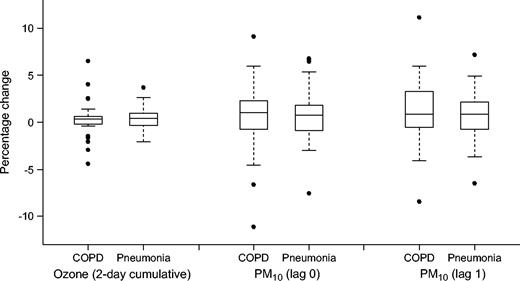
Table 2 shows the results of the meta-analysis across all cities based on the city-specific models in which the baseline matching scheme was used. Overall, during the warm season, there was an increase in hospital admissions associated with ozone exposure, specifically with such exposure on the day before. The 2-day cumulative effect of a 5-ppb increase in 8-hour ozone levels was a 0.27 percent (95 percent confidence interval (CI): 0.08, 0.47) increase in COPD admissions and a 0.41 percent (95 percent CI: 0.26, 0.57) increase in pneumonia admissions. The distribution of the city-specific estimates for the warm season is shown in figure 1, with the extreme values corresponding to those estimates with larger standard errors. Results from the meta-analysis showed that hospital admissions during the cold season decreased with increasing ozone concentrations, which resulted in a weak positive association for the full-year period. Results were very similar when other matching schemes were used. The increases in COPD and pneumonia admissions during the warm season, for instance, were 0.26 percent (95 percent CI: −0.05, 0.57) and 0.32 percent (95 percent CI: 0.12, 0.52), respectively, when additionally matching on temperature, and 0.30 percent (95 percent CI: 0.10, 0.51) and 0.48 percent (95 percent CI: 0.30, 0.67), respectively, when matching on day of the week. After we restricted the analysis to those days for which PM10 measurements were available, adjustment for PM10 did not substantially modify the results (not shown).
Distribution of the city-specific estimates of the percentage change in respiratory hospital admissions associated with air pollution during the warm season in 36 US cities during 1986–1999. Estimates are presented as the percentage increase in hospital admissions associated with a 5-ppb increase in ozone or a 10-μg/m3 increase in particulate matter with an aerodynamic diameter of ≤10 μm (PM10). COPD, chronic obstructive pulmonary disease.
Percentage change in respiratory hospital admissions associated with air pollution exposure across 36 US cities during 1986–1999*
. | COPD† . | . | . | . | . | . | Pneumonia . | . | . | . | . | . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | ||||||||||
. | % . | 95% CI† . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | ||||||||||
| Ozone‡ | −0.32 | −0.49, −0.15 | 0.33 | 0.19, 0.47 | 0.04 | −0.13, 0.20 | −0.23 | −0.32, −0.13 | 0.21 | 0.11, 0.30 | 0.30 | −0.12, 0.08 | ||||||||||
| Warm season | −0.25 | −0.46, −0.04 | 0.48 | 0.30, 0.66 | 0.27 | 0.08, 0.47 | 0.01 | −0.12, 0.13 | 0.42 | 0.29, 0.55 | 0.41 | 0.26, 0.57 | ||||||||||
| Cold season§ | −0.48 | −0.75, −0.21 | 0.14 | −0.13, 0.42 | −0.31 | −0.61, −0.01 | −0.61 | −0.85, −0.36 | −0.17 | −0.34, −0.004 | −0.83 | −1.13, −0.53 | ||||||||||
| PM10¶ | 0.29 | −0.01, 0.58 | 0.59 | 0.30, 0.88 | 0.45 | 0.27, 0.64 | 0.26 | 0.01, 0.52 | ||||||||||||||
| Warm season | 0.81 | 0.22, 1.41 | 1.47 | 0.93, 2.01 | 0.84 | 0.50, 1.19 | 0.79 | 0.45, 1.13 | ||||||||||||||
| Cold season | 0.06 | −0.40, 0.51 | 0.10 | −0.30, 0.49 | 0.30 | 0.07, 0.53 | 0.14 | −0.17, 0.45 | ||||||||||||||
. | COPD† . | . | . | . | . | . | Pneumonia . | . | . | . | . | . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | ||||||||||
. | % . | 95% CI† . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | ||||||||||
| Ozone‡ | −0.32 | −0.49, −0.15 | 0.33 | 0.19, 0.47 | 0.04 | −0.13, 0.20 | −0.23 | −0.32, −0.13 | 0.21 | 0.11, 0.30 | 0.30 | −0.12, 0.08 | ||||||||||
| Warm season | −0.25 | −0.46, −0.04 | 0.48 | 0.30, 0.66 | 0.27 | 0.08, 0.47 | 0.01 | −0.12, 0.13 | 0.42 | 0.29, 0.55 | 0.41 | 0.26, 0.57 | ||||||||||
| Cold season§ | −0.48 | −0.75, −0.21 | 0.14 | −0.13, 0.42 | −0.31 | −0.61, −0.01 | −0.61 | −0.85, −0.36 | −0.17 | −0.34, −0.004 | −0.83 | −1.13, −0.53 | ||||||||||
| PM10¶ | 0.29 | −0.01, 0.58 | 0.59 | 0.30, 0.88 | 0.45 | 0.27, 0.64 | 0.26 | 0.01, 0.52 | ||||||||||||||
| Warm season | 0.81 | 0.22, 1.41 | 1.47 | 0.93, 2.01 | 0.84 | 0.50, 1.19 | 0.79 | 0.45, 1.13 | ||||||||||||||
| Cold season | 0.06 | −0.40, 0.51 | 0.10 | −0.30, 0.49 | 0.30 | 0.07, 0.53 | 0.14 | −0.17, 0.45 | ||||||||||||||
Estimates are presented as percentage increase in hospital admissions associated with a 5-ppb increase in ozone or a 10-μg/m3 increase in particulate matter with an aerodynamic diameter of ≤10 μm (PM10).
COPD, chronic obstructive pulmonary disease; CI, confidence interval.
Estimates for ozone exposure at lag 0 and lag 1 were obtained by including both variables in the same model.
Estimates for ozone exposure during the cold season are based on 16 cities.
Estimates for PM10 exposure at lag 0 and lag 1 were obtained by using separate models for each lag.
Percentage change in respiratory hospital admissions associated with air pollution exposure across 36 US cities during 1986–1999*
. | COPD† . | . | . | . | . | . | Pneumonia . | . | . | . | . | . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | ||||||||||
. | % . | 95% CI† . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | ||||||||||
| Ozone‡ | −0.32 | −0.49, −0.15 | 0.33 | 0.19, 0.47 | 0.04 | −0.13, 0.20 | −0.23 | −0.32, −0.13 | 0.21 | 0.11, 0.30 | 0.30 | −0.12, 0.08 | ||||||||||
| Warm season | −0.25 | −0.46, −0.04 | 0.48 | 0.30, 0.66 | 0.27 | 0.08, 0.47 | 0.01 | −0.12, 0.13 | 0.42 | 0.29, 0.55 | 0.41 | 0.26, 0.57 | ||||||||||
| Cold season§ | −0.48 | −0.75, −0.21 | 0.14 | −0.13, 0.42 | −0.31 | −0.61, −0.01 | −0.61 | −0.85, −0.36 | −0.17 | −0.34, −0.004 | −0.83 | −1.13, −0.53 | ||||||||||
| PM10¶ | 0.29 | −0.01, 0.58 | 0.59 | 0.30, 0.88 | 0.45 | 0.27, 0.64 | 0.26 | 0.01, 0.52 | ||||||||||||||
| Warm season | 0.81 | 0.22, 1.41 | 1.47 | 0.93, 2.01 | 0.84 | 0.50, 1.19 | 0.79 | 0.45, 1.13 | ||||||||||||||
| Cold season | 0.06 | −0.40, 0.51 | 0.10 | −0.30, 0.49 | 0.30 | 0.07, 0.53 | 0.14 | −0.17, 0.45 | ||||||||||||||
. | COPD† . | . | . | . | . | . | Pneumonia . | . | . | . | . | . | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | Lag 0 . | . | Lag 1 . | . | 2-day cumulative estimates . | . | ||||||||||
. | % . | 95% CI† . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | ||||||||||
| Ozone‡ | −0.32 | −0.49, −0.15 | 0.33 | 0.19, 0.47 | 0.04 | −0.13, 0.20 | −0.23 | −0.32, −0.13 | 0.21 | 0.11, 0.30 | 0.30 | −0.12, 0.08 | ||||||||||
| Warm season | −0.25 | −0.46, −0.04 | 0.48 | 0.30, 0.66 | 0.27 | 0.08, 0.47 | 0.01 | −0.12, 0.13 | 0.42 | 0.29, 0.55 | 0.41 | 0.26, 0.57 | ||||||||||
| Cold season§ | −0.48 | −0.75, −0.21 | 0.14 | −0.13, 0.42 | −0.31 | −0.61, −0.01 | −0.61 | −0.85, −0.36 | −0.17 | −0.34, −0.004 | −0.83 | −1.13, −0.53 | ||||||||||
| PM10¶ | 0.29 | −0.01, 0.58 | 0.59 | 0.30, 0.88 | 0.45 | 0.27, 0.64 | 0.26 | 0.01, 0.52 | ||||||||||||||
| Warm season | 0.81 | 0.22, 1.41 | 1.47 | 0.93, 2.01 | 0.84 | 0.50, 1.19 | 0.79 | 0.45, 1.13 | ||||||||||||||
| Cold season | 0.06 | −0.40, 0.51 | 0.10 | −0.30, 0.49 | 0.30 | 0.07, 0.53 | 0.14 | −0.17, 0.45 | ||||||||||||||
Estimates are presented as percentage increase in hospital admissions associated with a 5-ppb increase in ozone or a 10-μg/m3 increase in particulate matter with an aerodynamic diameter of ≤10 μm (PM10).
COPD, chronic obstructive pulmonary disease; CI, confidence interval.
Estimates for ozone exposure at lag 0 and lag 1 were obtained by including both variables in the same model.
Estimates for ozone exposure during the cold season are based on 16 cities.
Estimates for PM10 exposure at lag 0 and lag 1 were obtained by using separate models for each lag.
As shown in table 2, there was also an overall increase in respiratory hospital admissions associated with PM10 concentrations throughout the year, with a more marked effect during the warm season. The between-city variability in the estimates for that season is presented in figure 1. Results from the meta-analysis showed that, for COPD, the larger increase during the warm season (1.47 percent for every 10-μg/m3 increase in PM10) was associated with PM10 exposure on the day before (lag 1); for pneumonia, the main increase (0.84 percent) occurred on the same day of exposure (lag 0). Repeating the analyses for the warm season matching also for apparent temperature led to similar results, with an increase of 1.30 percent (95 percent CI: 0.58, 2.02) in COPD admissions associated with PM10 at lag 1 and of 0.94 percent (95 percent CI: 0.41, 1.46) in pneumonia admissions associated with PM10 at lag 0. The associations remained unaltered when analyses were repeated adjusting for ozone (results not shown).
We further examined the potential for effect modification of the city characteristics presented in table 3. In general, all characteristics varied from city to city. The proportion of households with central air conditioning was especially variable, ranging from 6.2 percent in Seattle to 93.3 percent in Houston. Central air conditioning and poverty were more common in those cities with a higher summer apparent temperature (Spearman's r = 0.74 and r = 0.52, respectively) but were unrelated to the variance of summer apparent temperature (r = 0.07 and r = 0.23, respectively).
City characteristics included in the analysis of effect modification, United States, 1986–1999
City, state . | People aged ≥65 years . | . | Daily summer apparent temperature (°C) . | . | Percentage of households with central air conditioning . | Percentage of PM10* from traffic . | ||
|---|---|---|---|---|---|---|---|---|
| . | Percentage living in poverty . | Emphysema mortality rate (deaths/100,000) . | Mean . | Variance . | . | . | ||
| Albuquerque, New Mexico | 10.7 | 45.8 | 22.9 | 6.3 | 1.0 | |||
| Atlanta, Georgia | 13.7 | 58.7 | 29.0 | 10.5 | 82.6 | 2.8 | ||
| Baltimore, Maryland | 13.2 | 23.5 | 26.6 | 22.0 | 67.3 | 3.2 | ||
| Birmingham, Alabama | 18.3 | 29.5 | 29.5 | 10.9 | 70.2 | 1.5 | ||
| Boston, Massachusetts | 9.6 | 34.9 | 22.6 | 25.0 | 17.0 | 2.5 | ||
| Boulder, Colorado | 8.7 | 46.9 | 20.0 | 11.3 | 6.3 | 1.7 | ||
| Canton, Ohio | 8.7 | 49.5 | 22.6 | 23.1 | 29.9 | 2.3 | ||
| Chicago, Illinois | 11.2 | 34.3 | 23.7 | 29.6 | 43.2 | 5.0 | ||
| Cincinnati, Ohio | 11.2 | 29.3 | 25.4 | 20.7 | 66.2 | 3.5 | ||
| Cleveland, Ohio | 10.2 | 33.0 | 23.3 | 24.4 | 39.3 | 5.5 | ||
| Colorado Springs, Colorado | 8.1 | 65.5 | 18.2 | 10.6 | 13.4 | 1.6 | ||
| Columbus, Ohio | 10.3 | 61.0 | 24.7 | 22.7 | 63.7 | 3.4 | ||
| Denver, Colorado | 12.7 | 87.9 | 20.0 | 11.3 | 25.7 | 3.0 | ||
| Detroit, Michigan | 13.5 | 40.2 | 23.2 | 25.7 | 41.0 | 7.5 | ||
| Honolulu, Hawaii | 7.8 | 25.4 | 29.8 | 2.0 | 2.8 | |||
| Houston, Texas | 15.8 | 46.9 | 32.9 | 6.3 | 93.3 | 1.1 | ||
| Jersey City, New Jersey | 15.2 | 27.9 | 26.1 | 23.3 | 35.1 | 3.2 | ||
| Los Angeles, California | 9.2 | 28.4 | 20.7 | 6.2 | 32.1 | 11.7 | ||
| Minneapolis, Minnesota | 8.0 | 32.7 | 22.5 | 25.1 | 48.4 | 3.2 | ||
| Nashville, Tennessee | 14.5 | 63.9 | 28.7 | 14.7 | 72.2 | 2.5 | ||
| New Haven, Connecticut | 7.7 | 17.8 | 22.9 | 23.1 | 23.9 | 5.6 | ||
| New York City, New York | 16.5 | 17.2 | 25.6 | 22.1 | 11.1 | 2.4 | ||
| Palm Beach, Florida | 7.1 | 35.5 | 32.9 | 2.7 | 2.2 | |||
| Philadelphia, Pennsylvania | 16.3 | 19.9 | 26.6 | 23.5 | 38.8 | 3.5 | ||
| Pittsburgh, Pennsylvania | 10.1 | 34.9 | 23.2 | 21.3 | 33.4 | 5.0 | ||
| Provo, Utah | 6.7 | 38.4 | 22.2 | 17.4 | 26.9 | 2.2 | ||
| Sacramento, California | 6.8 | 46.3 | 22.2 | 13.1 | 71.7 | 5.6 | ||
| Salt Lake City, Utah | 7.8 | 42.0 | 22.2 | 17.4 | 39.7 | 2.8 | ||
| San Diego, California | 6.3 | 39.3 | 21.2 | 7.5 | 26.6 | 3.5 | ||
| San Francisco, California | 9.9 | 29.5 | 15.8 | 4.6 | 13.2 | 9.0 | ||
| Seattle, Washington | 7.3 | 34.7 | 16.7 | 12.1 | 6.2 | 3.0 | ||
| Steubenville, Ohio | 11.4 | 23.2 | 21.3 | 71.6 | 1.2 | |||
| St. Louis, Missouri | 10.7 | 37.5 | 28.2 | 24.0 | 76.5 | 1.7 | ||
| Spokane, Washington | 10.9 | 73.8 | 17.3 | 20.1 | 28.2 | 2.2 | ||
| Washington DC | 17.2 | 23.4 | 27.9 | 21.2 | 86.7 | 7.9 | ||
| Youngstown, Ohio | 11.3 | 43.6 | 21.8 | 23.7 | 22.8 | 3.0 | ||
| Median (25th, 75th percentiles) | 10.5 (8.0, 13.4) | 35.5 (29.3, 46.9) | 23.2 (21.9, 26.6) | 20.4 (10.6, 23.3) | 38.8 (24.8, 68.8) | 3.0 (2.2, 4.6) | ||
City, state . | People aged ≥65 years . | . | Daily summer apparent temperature (°C) . | . | Percentage of households with central air conditioning . | Percentage of PM10* from traffic . | ||
|---|---|---|---|---|---|---|---|---|
| . | Percentage living in poverty . | Emphysema mortality rate (deaths/100,000) . | Mean . | Variance . | . | . | ||
| Albuquerque, New Mexico | 10.7 | 45.8 | 22.9 | 6.3 | 1.0 | |||
| Atlanta, Georgia | 13.7 | 58.7 | 29.0 | 10.5 | 82.6 | 2.8 | ||
| Baltimore, Maryland | 13.2 | 23.5 | 26.6 | 22.0 | 67.3 | 3.2 | ||
| Birmingham, Alabama | 18.3 | 29.5 | 29.5 | 10.9 | 70.2 | 1.5 | ||
| Boston, Massachusetts | 9.6 | 34.9 | 22.6 | 25.0 | 17.0 | 2.5 | ||
| Boulder, Colorado | 8.7 | 46.9 | 20.0 | 11.3 | 6.3 | 1.7 | ||
| Canton, Ohio | 8.7 | 49.5 | 22.6 | 23.1 | 29.9 | 2.3 | ||
| Chicago, Illinois | 11.2 | 34.3 | 23.7 | 29.6 | 43.2 | 5.0 | ||
| Cincinnati, Ohio | 11.2 | 29.3 | 25.4 | 20.7 | 66.2 | 3.5 | ||
| Cleveland, Ohio | 10.2 | 33.0 | 23.3 | 24.4 | 39.3 | 5.5 | ||
| Colorado Springs, Colorado | 8.1 | 65.5 | 18.2 | 10.6 | 13.4 | 1.6 | ||
| Columbus, Ohio | 10.3 | 61.0 | 24.7 | 22.7 | 63.7 | 3.4 | ||
| Denver, Colorado | 12.7 | 87.9 | 20.0 | 11.3 | 25.7 | 3.0 | ||
| Detroit, Michigan | 13.5 | 40.2 | 23.2 | 25.7 | 41.0 | 7.5 | ||
| Honolulu, Hawaii | 7.8 | 25.4 | 29.8 | 2.0 | 2.8 | |||
| Houston, Texas | 15.8 | 46.9 | 32.9 | 6.3 | 93.3 | 1.1 | ||
| Jersey City, New Jersey | 15.2 | 27.9 | 26.1 | 23.3 | 35.1 | 3.2 | ||
| Los Angeles, California | 9.2 | 28.4 | 20.7 | 6.2 | 32.1 | 11.7 | ||
| Minneapolis, Minnesota | 8.0 | 32.7 | 22.5 | 25.1 | 48.4 | 3.2 | ||
| Nashville, Tennessee | 14.5 | 63.9 | 28.7 | 14.7 | 72.2 | 2.5 | ||
| New Haven, Connecticut | 7.7 | 17.8 | 22.9 | 23.1 | 23.9 | 5.6 | ||
| New York City, New York | 16.5 | 17.2 | 25.6 | 22.1 | 11.1 | 2.4 | ||
| Palm Beach, Florida | 7.1 | 35.5 | 32.9 | 2.7 | 2.2 | |||
| Philadelphia, Pennsylvania | 16.3 | 19.9 | 26.6 | 23.5 | 38.8 | 3.5 | ||
| Pittsburgh, Pennsylvania | 10.1 | 34.9 | 23.2 | 21.3 | 33.4 | 5.0 | ||
| Provo, Utah | 6.7 | 38.4 | 22.2 | 17.4 | 26.9 | 2.2 | ||
| Sacramento, California | 6.8 | 46.3 | 22.2 | 13.1 | 71.7 | 5.6 | ||
| Salt Lake City, Utah | 7.8 | 42.0 | 22.2 | 17.4 | 39.7 | 2.8 | ||
| San Diego, California | 6.3 | 39.3 | 21.2 | 7.5 | 26.6 | 3.5 | ||
| San Francisco, California | 9.9 | 29.5 | 15.8 | 4.6 | 13.2 | 9.0 | ||
| Seattle, Washington | 7.3 | 34.7 | 16.7 | 12.1 | 6.2 | 3.0 | ||
| Steubenville, Ohio | 11.4 | 23.2 | 21.3 | 71.6 | 1.2 | |||
| St. Louis, Missouri | 10.7 | 37.5 | 28.2 | 24.0 | 76.5 | 1.7 | ||
| Spokane, Washington | 10.9 | 73.8 | 17.3 | 20.1 | 28.2 | 2.2 | ||
| Washington DC | 17.2 | 23.4 | 27.9 | 21.2 | 86.7 | 7.9 | ||
| Youngstown, Ohio | 11.3 | 43.6 | 21.8 | 23.7 | 22.8 | 3.0 | ||
| Median (25th, 75th percentiles) | 10.5 (8.0, 13.4) | 35.5 (29.3, 46.9) | 23.2 (21.9, 26.6) | 20.4 (10.6, 23.3) | 38.8 (24.8, 68.8) | 3.0 (2.2, 4.6) | ||
PM10, particulate matter with an aerodynamic diameter of ≤10 μm.
City characteristics included in the analysis of effect modification, United States, 1986–1999
City, state . | People aged ≥65 years . | . | Daily summer apparent temperature (°C) . | . | Percentage of households with central air conditioning . | Percentage of PM10* from traffic . | ||
|---|---|---|---|---|---|---|---|---|
| . | Percentage living in poverty . | Emphysema mortality rate (deaths/100,000) . | Mean . | Variance . | . | . | ||
| Albuquerque, New Mexico | 10.7 | 45.8 | 22.9 | 6.3 | 1.0 | |||
| Atlanta, Georgia | 13.7 | 58.7 | 29.0 | 10.5 | 82.6 | 2.8 | ||
| Baltimore, Maryland | 13.2 | 23.5 | 26.6 | 22.0 | 67.3 | 3.2 | ||
| Birmingham, Alabama | 18.3 | 29.5 | 29.5 | 10.9 | 70.2 | 1.5 | ||
| Boston, Massachusetts | 9.6 | 34.9 | 22.6 | 25.0 | 17.0 | 2.5 | ||
| Boulder, Colorado | 8.7 | 46.9 | 20.0 | 11.3 | 6.3 | 1.7 | ||
| Canton, Ohio | 8.7 | 49.5 | 22.6 | 23.1 | 29.9 | 2.3 | ||
| Chicago, Illinois | 11.2 | 34.3 | 23.7 | 29.6 | 43.2 | 5.0 | ||
| Cincinnati, Ohio | 11.2 | 29.3 | 25.4 | 20.7 | 66.2 | 3.5 | ||
| Cleveland, Ohio | 10.2 | 33.0 | 23.3 | 24.4 | 39.3 | 5.5 | ||
| Colorado Springs, Colorado | 8.1 | 65.5 | 18.2 | 10.6 | 13.4 | 1.6 | ||
| Columbus, Ohio | 10.3 | 61.0 | 24.7 | 22.7 | 63.7 | 3.4 | ||
| Denver, Colorado | 12.7 | 87.9 | 20.0 | 11.3 | 25.7 | 3.0 | ||
| Detroit, Michigan | 13.5 | 40.2 | 23.2 | 25.7 | 41.0 | 7.5 | ||
| Honolulu, Hawaii | 7.8 | 25.4 | 29.8 | 2.0 | 2.8 | |||
| Houston, Texas | 15.8 | 46.9 | 32.9 | 6.3 | 93.3 | 1.1 | ||
| Jersey City, New Jersey | 15.2 | 27.9 | 26.1 | 23.3 | 35.1 | 3.2 | ||
| Los Angeles, California | 9.2 | 28.4 | 20.7 | 6.2 | 32.1 | 11.7 | ||
| Minneapolis, Minnesota | 8.0 | 32.7 | 22.5 | 25.1 | 48.4 | 3.2 | ||
| Nashville, Tennessee | 14.5 | 63.9 | 28.7 | 14.7 | 72.2 | 2.5 | ||
| New Haven, Connecticut | 7.7 | 17.8 | 22.9 | 23.1 | 23.9 | 5.6 | ||
| New York City, New York | 16.5 | 17.2 | 25.6 | 22.1 | 11.1 | 2.4 | ||
| Palm Beach, Florida | 7.1 | 35.5 | 32.9 | 2.7 | 2.2 | |||
| Philadelphia, Pennsylvania | 16.3 | 19.9 | 26.6 | 23.5 | 38.8 | 3.5 | ||
| Pittsburgh, Pennsylvania | 10.1 | 34.9 | 23.2 | 21.3 | 33.4 | 5.0 | ||
| Provo, Utah | 6.7 | 38.4 | 22.2 | 17.4 | 26.9 | 2.2 | ||
| Sacramento, California | 6.8 | 46.3 | 22.2 | 13.1 | 71.7 | 5.6 | ||
| Salt Lake City, Utah | 7.8 | 42.0 | 22.2 | 17.4 | 39.7 | 2.8 | ||
| San Diego, California | 6.3 | 39.3 | 21.2 | 7.5 | 26.6 | 3.5 | ||
| San Francisco, California | 9.9 | 29.5 | 15.8 | 4.6 | 13.2 | 9.0 | ||
| Seattle, Washington | 7.3 | 34.7 | 16.7 | 12.1 | 6.2 | 3.0 | ||
| Steubenville, Ohio | 11.4 | 23.2 | 21.3 | 71.6 | 1.2 | |||
| St. Louis, Missouri | 10.7 | 37.5 | 28.2 | 24.0 | 76.5 | 1.7 | ||
| Spokane, Washington | 10.9 | 73.8 | 17.3 | 20.1 | 28.2 | 2.2 | ||
| Washington DC | 17.2 | 23.4 | 27.9 | 21.2 | 86.7 | 7.9 | ||
| Youngstown, Ohio | 11.3 | 43.6 | 21.8 | 23.7 | 22.8 | 3.0 | ||
| Median (25th, 75th percentiles) | 10.5 (8.0, 13.4) | 35.5 (29.3, 46.9) | 23.2 (21.9, 26.6) | 20.4 (10.6, 23.3) | 38.8 (24.8, 68.8) | 3.0 (2.2, 4.6) | ||
City, state . | People aged ≥65 years . | . | Daily summer apparent temperature (°C) . | . | Percentage of households with central air conditioning . | Percentage of PM10* from traffic . | ||
|---|---|---|---|---|---|---|---|---|
| . | Percentage living in poverty . | Emphysema mortality rate (deaths/100,000) . | Mean . | Variance . | . | . | ||
| Albuquerque, New Mexico | 10.7 | 45.8 | 22.9 | 6.3 | 1.0 | |||
| Atlanta, Georgia | 13.7 | 58.7 | 29.0 | 10.5 | 82.6 | 2.8 | ||
| Baltimore, Maryland | 13.2 | 23.5 | 26.6 | 22.0 | 67.3 | 3.2 | ||
| Birmingham, Alabama | 18.3 | 29.5 | 29.5 | 10.9 | 70.2 | 1.5 | ||
| Boston, Massachusetts | 9.6 | 34.9 | 22.6 | 25.0 | 17.0 | 2.5 | ||
| Boulder, Colorado | 8.7 | 46.9 | 20.0 | 11.3 | 6.3 | 1.7 | ||
| Canton, Ohio | 8.7 | 49.5 | 22.6 | 23.1 | 29.9 | 2.3 | ||
| Chicago, Illinois | 11.2 | 34.3 | 23.7 | 29.6 | 43.2 | 5.0 | ||
| Cincinnati, Ohio | 11.2 | 29.3 | 25.4 | 20.7 | 66.2 | 3.5 | ||
| Cleveland, Ohio | 10.2 | 33.0 | 23.3 | 24.4 | 39.3 | 5.5 | ||
| Colorado Springs, Colorado | 8.1 | 65.5 | 18.2 | 10.6 | 13.4 | 1.6 | ||
| Columbus, Ohio | 10.3 | 61.0 | 24.7 | 22.7 | 63.7 | 3.4 | ||
| Denver, Colorado | 12.7 | 87.9 | 20.0 | 11.3 | 25.7 | 3.0 | ||
| Detroit, Michigan | 13.5 | 40.2 | 23.2 | 25.7 | 41.0 | 7.5 | ||
| Honolulu, Hawaii | 7.8 | 25.4 | 29.8 | 2.0 | 2.8 | |||
| Houston, Texas | 15.8 | 46.9 | 32.9 | 6.3 | 93.3 | 1.1 | ||
| Jersey City, New Jersey | 15.2 | 27.9 | 26.1 | 23.3 | 35.1 | 3.2 | ||
| Los Angeles, California | 9.2 | 28.4 | 20.7 | 6.2 | 32.1 | 11.7 | ||
| Minneapolis, Minnesota | 8.0 | 32.7 | 22.5 | 25.1 | 48.4 | 3.2 | ||
| Nashville, Tennessee | 14.5 | 63.9 | 28.7 | 14.7 | 72.2 | 2.5 | ||
| New Haven, Connecticut | 7.7 | 17.8 | 22.9 | 23.1 | 23.9 | 5.6 | ||
| New York City, New York | 16.5 | 17.2 | 25.6 | 22.1 | 11.1 | 2.4 | ||
| Palm Beach, Florida | 7.1 | 35.5 | 32.9 | 2.7 | 2.2 | |||
| Philadelphia, Pennsylvania | 16.3 | 19.9 | 26.6 | 23.5 | 38.8 | 3.5 | ||
| Pittsburgh, Pennsylvania | 10.1 | 34.9 | 23.2 | 21.3 | 33.4 | 5.0 | ||
| Provo, Utah | 6.7 | 38.4 | 22.2 | 17.4 | 26.9 | 2.2 | ||
| Sacramento, California | 6.8 | 46.3 | 22.2 | 13.1 | 71.7 | 5.6 | ||
| Salt Lake City, Utah | 7.8 | 42.0 | 22.2 | 17.4 | 39.7 | 2.8 | ||
| San Diego, California | 6.3 | 39.3 | 21.2 | 7.5 | 26.6 | 3.5 | ||
| San Francisco, California | 9.9 | 29.5 | 15.8 | 4.6 | 13.2 | 9.0 | ||
| Seattle, Washington | 7.3 | 34.7 | 16.7 | 12.1 | 6.2 | 3.0 | ||
| Steubenville, Ohio | 11.4 | 23.2 | 21.3 | 71.6 | 1.2 | |||
| St. Louis, Missouri | 10.7 | 37.5 | 28.2 | 24.0 | 76.5 | 1.7 | ||
| Spokane, Washington | 10.9 | 73.8 | 17.3 | 20.1 | 28.2 | 2.2 | ||
| Washington DC | 17.2 | 23.4 | 27.9 | 21.2 | 86.7 | 7.9 | ||
| Youngstown, Ohio | 11.3 | 43.6 | 21.8 | 23.7 | 22.8 | 3.0 | ||
| Median (25th, 75th percentiles) | 10.5 (8.0, 13.4) | 35.5 (29.3, 46.9) | 23.2 (21.9, 26.6) | 20.4 (10.6, 23.3) | 38.8 (24.8, 68.8) | 3.0 (2.2, 4.6) | ||
PM10, particulate matter with an aerodynamic diameter of ≤10 μm.
The association between hospital admissions and air pollution during the warm season was modified by some of the city characteristics (table 4). Overall, in cities with a large proportion of households with central air conditioning, the effect of air pollution on hospital admissions was milder, especially for pneumonia admissions. For instance, in a city with a low proportion of central air conditioning (in the 25th percentile of the distribution), the estimated percentage increase in pneumonia admissions for every 10-μg/m3 increase in PM10 was 1.47 percent; whereas, in a city with a high proportion of central air conditioning (in the 75th percentile), the change in pneumonia admissions was negligible (−0.11 percent). The effect of air pollution was consistently lower for those cities with a higher summer apparent temperature, although the interaction was statistically significant for the association between PM10 and pneumonia admissions only and disappeared after adjusting for percentage of central air conditioning (p = 0.96, results not shown). Similarly, the milder effect of PM10 on cities with a large proportion of people living in poverty disappeared after adjusting for percentage of central air conditioning (p = 0.38, results not shown). The variability of summer apparent temperature modified the effect of ozone on COPD (about a fourfold decrease when the 25th percentile was compared with the 75th percentile) and remained the same after adjustment for other city characteristics. When we examined modification of the association between PM10 and hospital admissions for the entire year, we obtained results similar to the ones presented in table 4 but weaker associations (results not shown).
Modification by city characteristics of the effect of air pollution on hospital admissions in 36 US cities during 1986–1999: comparison of the predicted percentage change in hospital admissions at the 25th and the 75th percentiles of the effect-modifier distribution†
. | Ozone exposure in the warm season‡ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD§ admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
. | % . | 95% CI§ . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 0.38 | 0.06, 0.70 | 0.24 | 0.04, 0.45 | 0.50 | 0.24, 0.76 | 0.38 | 0.21, 0.55 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 0.28 | 0.08, 0.49 | 0.20 | −0.10, 0.49 | 0.47 | 0.33, 0.61 | 0.32 | 0.12, 0.53 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 0.29 | 0.04, 0.54 | 0.26 | 0.05, 0.48 | 0.51 | 0.31, 0.72 | 0.36 | 0.19, 0.53 | |||||||
| Variance | 0.45* | 0.20, 0.70 | 0.12* | −0.12, 0.36 | 0.42 | 0.21, 0.63 | 0.40 | 0.21, 0.59 | |||||||
| Percentage of households with central air conditioning | 0.29 | 0.04, 0.53 | 0.23 | −0.05, 0.51 | 0.54* | 0.38, 0.70 | 0.30* | 0.10, 0.49 | |||||||
. | Ozone exposure in the warm season‡ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD§ admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
. | % . | 95% CI§ . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 0.38 | 0.06, 0.70 | 0.24 | 0.04, 0.45 | 0.50 | 0.24, 0.76 | 0.38 | 0.21, 0.55 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 0.28 | 0.08, 0.49 | 0.20 | −0.10, 0.49 | 0.47 | 0.33, 0.61 | 0.32 | 0.12, 0.53 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 0.29 | 0.04, 0.54 | 0.26 | 0.05, 0.48 | 0.51 | 0.31, 0.72 | 0.36 | 0.19, 0.53 | |||||||
| Variance | 0.45* | 0.20, 0.70 | 0.12* | −0.12, 0.36 | 0.42 | 0.21, 0.63 | 0.40 | 0.21, 0.59 | |||||||
| Percentage of households with central air conditioning | 0.29 | 0.04, 0.53 | 0.23 | −0.05, 0.51 | 0.54* | 0.38, 0.70 | 0.30* | 0.10, 0.49 | |||||||
| . | PM10 exposure in the warm season¶ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
| . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 1.61 | 0.65, 2.58 | 1.40 | 0.69, 2.11 | 1.37* | 0.77, 1.98 | 0.52* | 0.06, 0.98 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 1.78** | 1.10, 2.46 | 1.03** | 0.30, 1.77 | 0.91 | 0.49, 1.32 | 0.85 | 0.39, 1.31 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 1.56 | 0.91, 2.22 | 1.33 | 0.52, 2.13 | 1.13* | 0.71, 1.54 | 0.37* | −0.15, 0.88 | |||||||
| Variance | 0.96 | −0.27, 2.19 | 1.53 | 0.95, 2.12 | 1.07 | 0.33, 1.80 | 0.84 | 0.50, 1.19 | |||||||
| Percentage of households with central air conditioning | 1.74 | 0.92, 2.55 | 1.07 | 0.03, 2.12 | 1.47* | 0.94, 2.00 | −0.11* | −0.79, 0.57 | |||||||
| Percentage of PM10 from traffic | 1.37 | 0.53, 2.20 | 1.47 | 0.93, 2.00 | 0.53 | −0.01, 1.06 | 0.83 | 0.49, 1.18 | |||||||
| . | PM10 exposure in the warm season¶ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
| . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 1.61 | 0.65, 2.58 | 1.40 | 0.69, 2.11 | 1.37* | 0.77, 1.98 | 0.52* | 0.06, 0.98 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 1.78** | 1.10, 2.46 | 1.03** | 0.30, 1.77 | 0.91 | 0.49, 1.32 | 0.85 | 0.39, 1.31 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 1.56 | 0.91, 2.22 | 1.33 | 0.52, 2.13 | 1.13* | 0.71, 1.54 | 0.37* | −0.15, 0.88 | |||||||
| Variance | 0.96 | −0.27, 2.19 | 1.53 | 0.95, 2.12 | 1.07 | 0.33, 1.80 | 0.84 | 0.50, 1.19 | |||||||
| Percentage of households with central air conditioning | 1.74 | 0.92, 2.55 | 1.07 | 0.03, 2.12 | 1.47* | 0.94, 2.00 | −0.11* | −0.79, 0.57 | |||||||
| Percentage of PM10 from traffic | 1.37 | 0.53, 2.20 | 1.47 | 0.93, 2.00 | 0.53 | −0.01, 1.06 | 0.83 | 0.49, 1.18 | |||||||
Two-sided p < 0.05 in the meta-regression model; **two-sided p < 0.1 in the meta-regression model.
Estimates are presented as percentage increase in hospital admissions associated with a 5-ppb increase in ozone or a 10-μg/m3 increase in particulate matter with an aerodynamic diameter of ≤10 μm (PM10).
Modification of the association between ozone during the warm season and hospital admissions was examined by using the 2-day cumulative-effect models.
COPD, chronic obstructive pulmonary disease; CI, confidence interval.
Modification of the association between PM10 during the warm season and hospital admissions was examined by using the lag 1 model for COPD admissions and the lag 0 model for pneumonia admissions.
Modification by city characteristics of the effect of air pollution on hospital admissions in 36 US cities during 1986–1999: comparison of the predicted percentage change in hospital admissions at the 25th and the 75th percentiles of the effect-modifier distribution†
. | Ozone exposure in the warm season‡ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD§ admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
. | % . | 95% CI§ . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 0.38 | 0.06, 0.70 | 0.24 | 0.04, 0.45 | 0.50 | 0.24, 0.76 | 0.38 | 0.21, 0.55 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 0.28 | 0.08, 0.49 | 0.20 | −0.10, 0.49 | 0.47 | 0.33, 0.61 | 0.32 | 0.12, 0.53 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 0.29 | 0.04, 0.54 | 0.26 | 0.05, 0.48 | 0.51 | 0.31, 0.72 | 0.36 | 0.19, 0.53 | |||||||
| Variance | 0.45* | 0.20, 0.70 | 0.12* | −0.12, 0.36 | 0.42 | 0.21, 0.63 | 0.40 | 0.21, 0.59 | |||||||
| Percentage of households with central air conditioning | 0.29 | 0.04, 0.53 | 0.23 | −0.05, 0.51 | 0.54* | 0.38, 0.70 | 0.30* | 0.10, 0.49 | |||||||
. | Ozone exposure in the warm season‡ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD§ admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
. | % . | 95% CI§ . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 0.38 | 0.06, 0.70 | 0.24 | 0.04, 0.45 | 0.50 | 0.24, 0.76 | 0.38 | 0.21, 0.55 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 0.28 | 0.08, 0.49 | 0.20 | −0.10, 0.49 | 0.47 | 0.33, 0.61 | 0.32 | 0.12, 0.53 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 0.29 | 0.04, 0.54 | 0.26 | 0.05, 0.48 | 0.51 | 0.31, 0.72 | 0.36 | 0.19, 0.53 | |||||||
| Variance | 0.45* | 0.20, 0.70 | 0.12* | −0.12, 0.36 | 0.42 | 0.21, 0.63 | 0.40 | 0.21, 0.59 | |||||||
| Percentage of households with central air conditioning | 0.29 | 0.04, 0.53 | 0.23 | −0.05, 0.51 | 0.54* | 0.38, 0.70 | 0.30* | 0.10, 0.49 | |||||||
| . | PM10 exposure in the warm season¶ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
| . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 1.61 | 0.65, 2.58 | 1.40 | 0.69, 2.11 | 1.37* | 0.77, 1.98 | 0.52* | 0.06, 0.98 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 1.78** | 1.10, 2.46 | 1.03** | 0.30, 1.77 | 0.91 | 0.49, 1.32 | 0.85 | 0.39, 1.31 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 1.56 | 0.91, 2.22 | 1.33 | 0.52, 2.13 | 1.13* | 0.71, 1.54 | 0.37* | −0.15, 0.88 | |||||||
| Variance | 0.96 | −0.27, 2.19 | 1.53 | 0.95, 2.12 | 1.07 | 0.33, 1.80 | 0.84 | 0.50, 1.19 | |||||||
| Percentage of households with central air conditioning | 1.74 | 0.92, 2.55 | 1.07 | 0.03, 2.12 | 1.47* | 0.94, 2.00 | −0.11* | −0.79, 0.57 | |||||||
| Percentage of PM10 from traffic | 1.37 | 0.53, 2.20 | 1.47 | 0.93, 2.00 | 0.53 | −0.01, 1.06 | 0.83 | 0.49, 1.18 | |||||||
| . | PM10 exposure in the warm season¶ . | . | . | . | . | . | . | . | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | Change in COPD admissions at the . | . | . | . | Change in pneumonia admissions at the . | . | . | . | |||||||
| . | 25th percentile . | . | 75th percentile . | . | 25th percentile . | . | 75th percentile . | . | |||||||
| . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | % . | 95% CI . | |||||||
| Percentage of people aged ≥65 years living in poverty | 1.61 | 0.65, 2.58 | 1.40 | 0.69, 2.11 | 1.37* | 0.77, 1.98 | 0.52* | 0.06, 0.98 | |||||||
| Emphysema mortality rate for people aged ≥65 years (deaths/100,000) | 1.78** | 1.10, 2.46 | 1.03** | 0.30, 1.77 | 0.91 | 0.49, 1.32 | 0.85 | 0.39, 1.31 | |||||||
| Daily summer apparent temperature (°C) | |||||||||||||||
| Mean | 1.56 | 0.91, 2.22 | 1.33 | 0.52, 2.13 | 1.13* | 0.71, 1.54 | 0.37* | −0.15, 0.88 | |||||||
| Variance | 0.96 | −0.27, 2.19 | 1.53 | 0.95, 2.12 | 1.07 | 0.33, 1.80 | 0.84 | 0.50, 1.19 | |||||||
| Percentage of households with central air conditioning | 1.74 | 0.92, 2.55 | 1.07 | 0.03, 2.12 | 1.47* | 0.94, 2.00 | −0.11* | −0.79, 0.57 | |||||||
| Percentage of PM10 from traffic | 1.37 | 0.53, 2.20 | 1.47 | 0.93, 2.00 | 0.53 | −0.01, 1.06 | 0.83 | 0.49, 1.18 | |||||||
Two-sided p < 0.05 in the meta-regression model; **two-sided p < 0.1 in the meta-regression model.
Estimates are presented as percentage increase in hospital admissions associated with a 5-ppb increase in ozone or a 10-μg/m3 increase in particulate matter with an aerodynamic diameter of ≤10 μm (PM10).
Modification of the association between ozone during the warm season and hospital admissions was examined by using the 2-day cumulative-effect models.
COPD, chronic obstructive pulmonary disease; CI, confidence interval.
Modification of the association between PM10 during the warm season and hospital admissions was examined by using the lag 1 model for COPD admissions and the lag 0 model for pneumonia admissions.
DISCUSSION
In a large, multicity study, we found effects of ozone and PM10 on hospital admissions for COPD and pneumonia and identified several city characteristics as effect modifiers. We found increased risks of COPD and pneumonia admissions associated with ambient ozone and PM10 levels, predominantly during the warm season. The proportion of households with central air conditioning was the most important effect modifier in that season. The variance of summer apparent temperature was associated with a milder effect of ozone on COPD.
Most of the literature about ozone effects on respiratory hospital admissions is based on data from single cities (6). One of the strengths of our study is that we included a large number of cities across the United States involving great diversity in weather, geography, and other characteristics that enabled us to analyze how these characteristics may modify the effect of air pollution. In addition, we analyzed more years of follow-up than previous multicity studies on the respiratory effects of ozone (3, 7, 24) and PM10 (25, 26). These two circumstances provided us with a larger sample size and more stable estimates than prior investigations offered.
In our study, we found that the risk of daily hospital admissions for COPD and for pneumonia increased with ozone concentration during the warm season but not during the cold season. Consistently, epidemiologic studies conducted in the United States and in other industrialized countries have also found an increased risk of both respiratory hospital admissions (3, 27) and total mortality (18, 28) associated with ozone exposure during the warm season only. Differences in the effect of ozone during these two seasons could be explained by the higher ozone concentrations and the larger amount of time spent outdoors during the warm season (29). In addition, ozone is a highly reactive gas whose indoor concentrations are extremely low in buildings with low ventilation (closed windows, etc.), which occurs more often in the winter. In the summer, open windows can result in some indoor exposure as well, and this exposure difference could also partially explain why positive effects are seen during the warm season only.
We also found an increased risk of COPD and pneumonia admissions associated with PM10 levels, which closely agrees with findings by Zanobetti et al. (2) using data from 10 US cities and also with results from the APHEA-2 study in eight European cities (26). The effect of PM10 on respiratory admissions was evident throughout the year but was stronger during the warm season. Because PM10 levels are usually similar during the warm and cold seasons, few studies have examined the effect of PM10 separately for these two seasons. A stronger effect during the warm season may be related to an increase in individual exposure (i.e., more time spent outdoors, higher ventilation rates, etc.) rather than to an overall increase in the outdoor ambient concentration. These results are consistent with those of Peng et al. (30), who recently reported that the effect of PM10 on mortality was higher in the summer. In our study, exposure to PM10 seemed to have an earlier effect on pneumonia admissions, occurring predominantly on the same day of exposure, than on COPD admissions, occurring predominantly 1 day after the exposure. An earlier effect of PM10 on pneumonia than on COPD was also observed in a mortality study of 20 US cities (31) and could be due to differences in the biologic mechanisms involved in the aggravation of these two respiratory disorders.
The effect of air pollution on respiratory hospital admissions was smaller in those cities with a larger proportion of central air conditioning. In a meta-analysis of 14 US cities, Janssen et al. (9) studied the role of air conditioning as an effect modifier of the relation between PM10 and hospital admissions and found a smaller effect for COPD, and possibly pneumonia, in cities with a larger proportion of central air conditioning. Several studies have shown that homes with air conditioning typically have lower exchange rates than homes that use open windows for ventilation (32, 33), suggesting a higher penetration of outdoor pollutants in homes without air conditioning. Therefore, those living in a home with central air conditioning are likely to be less exposed to outdoor air pollutants, resulting in attenuation of the association between ambient air pollution and health effects.
We observed a milder effect of ozone on COPD admissions during the warm season for those cities with a large variability in their summer temperature. Levels of ozone are generally related to temperature (18); thus, cities with a variable summer temperature are expected to also have more variable ozone levels. In our study, the variance of summer temperature was significantly correlated with the variance of ozone levels during the warm season (Spearman's r = 0.41). Therefore, a possible explanation for the observed effect modification would be that persons with COPD are more likely to be affected by high ozone concentrations when high levels have been sustained for several consecutive days. However, we did not find a statistically significant effect modification by ozone variability in our study (p = 0.20, results not shown), suggesting that there must also be other explanations for the interaction between ozone and variance of summer temperature.
Our results suggest that the observed interaction between PM10 and both the percentage of poverty and the mean summer apparent temperature may be explained by the high correlation of these variables with the proportion of central air conditioning rather than effect modification by the variables themselves. Although air pollution may affect different sociodemographic groups in different ways, in a study conducted in 14 US cities, the association between PM10 and respiratory hospital admissions was not modified by the percentage of poverty or by the percentage of non-White population (8). However, both the latter study and our study used county-level data, which may be too ecologic to be meaningful given that variation in socioeconomic status may be larger within a county than between counties.
In this study, the percentage of PM10 from traffic did not modify the risk of respiratory admissions due to PM10. Two different studies in the United States showed that PM10 from traffic (31) and particulate matter with an aerodynamic diameter of ≤2.5 μm (PM2.5) from mobile sources (34) were associated with a higher mortality risk than particulate matter from other sources. However, one of these studies (34) looked at cause-specific mortality and found no adverse effects of PM2.5 from mobile sources for deaths due to COPD or pneumonia. In a morbidity study in 14 US cities, a higher proportion of PM10 from traffic was marginally significantly associated with a stronger effect of PM10 on pneumonia admissions but not on COPD admissions (9).
The mechanisms behind the adverse respiratory effects of exposure to ozone and PM10 are unclear. Some authors have suggested that air pollution may act as an irritant and induce defensive responses in the airways, such as increased mucus secretion and increased bronchial hyperreactivity (35). Both ozone (36) and PM10 (37) are potent oxidants that have been shown to produce free radicals and oxidative stress on lung cells. Experimental chamber studies have shown decrements in forced expiratory volume in 1 second (FEV1) after exposure to ozone (38), but large interindividual differences have been observed in the responsiveness of both healthy subjects and those with COPD (27). Animal studies have shown an increased vulnerability to PM10 in animals with cardiopulmonary disease (39) and exacerbations of ongoing pneumococcal infection after exposure to concentrated ambient PM2.5 (40). Exposure to concentrated air particles has also been shown in vivo to increase reactive oxygen species in the lung (41).
The results presented here are unlikely to be due to inadequate control for weather and temporal trends, given that the results from the sensitivity analysis using alternative matching schemes (including control days matched on temperature) showed very similar associations. Confounding by individual characteristics is also unlikely because case-crossover sampling matches perfectly on individual characteristics (10–12). In our study, we did not address confounding by other air pollutants because of previous evidence that the effect of PM10 (2) and ozone (3) on respiratory hospital admissions remains practically unaltered after adjusting for other gaseous pollutants. A limitation of our study is that we used ambient air pollution as a surrogate for personal exposure, which may have resulted in a measurement error. Nevertheless, a recent article suggested that this measurement error would generally tend to bias estimates downward (25). Because of the irregular sampling scheme for PM10, we could not assess the cumulative effect of PM10 exposure, which may have led to either an overestimation or an underestimation of the risk estimates for each lag. Finally, although the emission estimates from the Environmental Protection Agency should be a reasonable indicator of the actual composition of ambient PM10 (9), they may have changed throughout the study period. The same is applicable to data on the percentage of central air conditioning, which was estimated by using data from a population sample during several different years.
In summary, our study confirmed, in a considerably larger sample of cities than, to our knowledge, has been previously examined, that short-term increases in PM10 and ozone ambient concentrations are related to hospital admissions for COPD and pneumonia, especially during the warm season. Our findings suggest that some city characteristics modify the effect of air pollution on respiratory hospital admissions. In particular, we found evidence that use of central air conditioning decreases the effect of air pollution and that variability of summer apparent temperature decreases the effect of ozone on COPD. On the other hand, we did not find evidence of a higher toxicity of PM10 from traffic as other studies observed for cardiovascular diseases (9, 34).
This study was funded by Environmental Protection Agency grant R-82735301-7 and National Institute of Environmental Health Sciences grant EH-0002.
Conflict of interest: none declared.
References
Pope CA 3rd, Dockery DW, Schwartz J. Review of epidemiological evidence of health effects of particulate air pollution.
Zanobetti A, Schwartz J, Dockery DW. Airborne particles are a risk factor for hospital admissions for heart and lung disease.
Burnett RT, Brook JR, Yung WT, et al. Association between ozone and hospitalization for respiratory diseases in 16 Canadian cities.
Health effects of outdoor air pollution. Committee of the Environmental and Occupational Health Assembly of the American Thoracic Society.
Roth HD, Hwang PM, Li Y. Assessment of recent ozone short-term epidemiologic studies.
Spix C, Anderson HR, Schwartz J, et al. Short-term effects of air pollution on hospital admissions of respiratory diseases in Europe: a quantitative summary of APHEA study results. Air Pollution and Health: a European Approach.
Samet JM, Zeger SL, Dominici F, et al. The National Morbidity, Mortality, and Air Pollution Study. Part II: morbidity and mortality from air pollution in the United States.
Janssen NA, Schwartz J, Zanobetti A, et al. Air conditioning and source-specific particles as modifiers of the effect of PM10 on hospital admissions for heart and lung disease.
Maclure M. The case-crossover design: a method for studying transient effects on the risk of acute events.
Bateson TF, Schwartz J. Control for seasonal variation and time trend in case-crossover studies of acute effects of environmental exposures.
Bateson TF, Schwartz J. Selection bias and confounding in case-crossover analyses of environmental time-series data.
Levy D, Lumley T, Sheppard L, et al. Referent selection in case-crossover analyses of acute health effects of air pollution.
Schwartz J, Zanobetti A, Bateson T. Morbidity and mortality among elderly residents of cities with daily PM measurements. In: Revised analyses of time-series studies of air pollution and health. Special report. Boston, MA: Health Effects Institute,
Nehls GJ Akland GG. Procedures for handling aerometric data.
Schwartz J. Assessing confounding, effect modification, and thresholds in the association between ambient particles and daily deaths.
Schwartz J. Is the association of airborne particles with daily deaths confounded by gaseous air pollutants? An approach to control by matching.
Schwartz J. How sensitive is the association between ozone and daily deaths to control for temperature?
Kalkstein LS, Valimont KM. An evaluation of summer discomfort in the United States using a relative climatological index.
Steadman RG. The assessment of sultriness. Part II: effects of wind, extra radiation and barometric pressure on apparent temperature.
US Census Bureau. The American Housing Survey. Washington, DC: Department of Housing and Urban Development,
US Environmental Protection Agency. Emissions and air quality data. County emission summary by source category,
Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods.
Thurston GD, Ito K, Kinney PL, et al. A multi-year study of air pollution and respiratory hospital admissions in three New York State metropolitan areas: results for 1988 and 1989 summers.
Samet JM, Dominici F, Zeger SL, et al. The National Morbidity, Mortality, and Air Pollution Study. Part I: methods and methodologic issues.
Atkinson RW, Anderson HR, Sunyer J, et al. Acute effects of particulate air pollution on respiratory admissions: results from APHEA 2 project. Air Pollution and Health: a European Approach.
Anderson HR, Spix C, Medina S, et al. Air pollution and daily admissions for chronic obstructive pulmonary disease in 6 European cities: results from the APHEA project.
Samet JM, Dominici F, Curriero FC, et al. Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994.
Burnett RT, Dales RE, Raizenne ME, et al. Effects of low ambient levels of ozone and sulfates on the frequency of respiratory admissions to Ontario hospitals.
Peng RD, Dominici F, Pastor-Barriuso R, et al. Seasonal analyses of air pollution and mortality in 100 US cities.
Zeka A, Zanobetti A, Schwartz J. Short-term effects of particulate matter on cause specific mortality: effects of lags and modification by city characteristics.
Suh HH, Spengler JD, Koutrakis P. Personal exposures to acid aerosols and ammonia.
Laden F, Neas LM, Dockery DW, et al. Association of fine particulate matter from different sources with daily mortality in six U.S. cities.
Anderson HR, Atkinson RW, Bremner SA, et al. Particulate air pollution and hospital admissions for cardiorespiratory diseases: are the elderly at greater risk?
Corradi M, Alinovi R, Goldoni M, et al. Biomarkers of oxidative stress after controlled human exposure to ozone.
Gilmour PS, Rahman I, Donaldson K, et al. Histone acetylation regulates epithelial IL-8 release mediated by oxidative stress from environmental particles.
McDonnell WF, Stewart PW, Andreoni S, et al. Prediction of ozone-induced FEV1 changes. Effects of concentration, duration, and ventilation.
Costa DL, Dreher KL. Bioavailable transition metals in particulate matter mediate cardiopulmonary injury in healthy and compromised animal models.
Zelikoff JT, Chen LC, Cohen MD, et al. Effects of inhaled ambient particulate matter on pulmonary antimicrobial immune defense.