Abstract
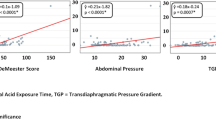
Gastroesophageal reflux disease (GERD) often is associated with pulmonary problems such as asthma as well as recurrent and nocturnal cough. Dual-probe 24-hr pH monitoring may assist in establishing a correlation between these symptoms and GERD-related symptoms. To determine if any specific symptom was predictive of aspiration, this study was undertaken. Ambulatory dual-probe esophageal pH monitoring was performed on 133 patients who had upper airway and additional symptoms for GERD. All patients had esophageal manometric studies of the lower esophageal sphincter (LES), the upper esophageal sphincter (UES), and the esophageal body before dual-probe pH monitoring was performed. Using two assembled glass probes, the distal and the proximal sensors were placed 5 cm above the proximal border of the LES and 1 cm below the lower border of the UES, respectively. Patients were classified into three groups: proximal and distal probe positive (group I), proximal probe negative and distal probe positive (group II) and proximal and distal probe negative (Group III) Upper airway and additional symptoms plus manometry results of the LES, body and UES study were compared between groups. In addition, positive distal probe patients (groups I and II) were compared for distal fraction of time at pH < 4 and number of reflux episodes at each probe position. A positive distal probe result was defined as an abnormal DeMeester score (>14.8). A proximal probe test result was considered positive if percent time pH < 4.0 was >1.1 for total, 1.7 for upright, and 0.6 for supine positions. The ages of the subjects ranged from 18 to 83 years (mean age: 50.5 ± 1.5 years). Groups I, II, and III included 16 patients, 38 patients, and 79 patients, respectively. Group I had a significantly higher incidence of nocturnal cough than the other two groups. (P < 0.05). The manometric data revealed between groups that LES pressure (LESP) for groups I and II was significantly lower than LESP for group III (P = 0.003). Cricoid pressure, pharyngeal pressure, length, and relaxation of UES were not different between groups. Fraction of reflux time for group I was significantly higher than for group II in the supine position and at mealtime (P < 0.05). The number of reflux episodes for group I was significantly higher at meal time (P < 0.01). In conclusion, nocturnal cough is strongly predictive of proximal esophageal reflux. Proximal reflux episodes are significantly more frequent in the supine position and correlate well with the high predictive value of nocturnal cough.
Similar content being viewed by others
REFERENCES
Mendelson CL: The aspiration of stomach contents into the lungs during obstetrics anesthesia. Am J Obstet Gynecol 52:191–205, 1946
Pellegrini CA, DeMeester TR, Johnson LF, Skinner DB: Gastroesophageal reflux and pulmonary aspiration: Incidence, functional abnormality, and results of surgical therapy. Surgery 86:110–119, 1979
Harding SM, Richter JE, Guzzo MR, Schan CA, Alexander RW, Bradley LA: Asthma and gastroesophageal reflux: Acid suppressive therapy improves asthma outcome. Am J Med 100:395–405, 1996
Koufman JA: The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): A clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope 101:1–64, 1991
DeMeester TR, Binavina L, lascone C, Courtney JV, Skinner DB: Chronic respiratory symptoms and occult gastroesophageal reflux. Ann Surg 210:337–345, 1990
Vaezi MF, Schroeder PL, Richter JE: Reproducibility of proximal probe pH parameters in 24-hour ambulatory pH monitoring. Am J Gastroenterol 92:825–829, 1997
Richter JE, Bradley LA, DeMeester TR, Wallace C: Normal 24-hour ambulatory esophageal pH values: Influence of study center, pH electrode, age, and gender. Dig Dis Sci 37:849–856, 1992
Gastal OL, Castell JA, Castel DO: Frequency and site of gastroesophageal reflux in patients with chest symptoms: Studies using proximal and distal pH monitoring. Chest 106:1793–1796, 1994
Paterson WG, Murat BW: Combined ambulatory esophageal manometry and dual probe pH-metry in evaluation of patients with chronic unexplained cough. Dig Dis Sci 39:1117–1125, 1994
Jacob P, Kahrilas PJ, Herzon G: Proximal esophageal pHmetry in patients with “reflux laryngitis'. ” Gastroenterology 100:305–310, 1991
Dobhan R, Castell DO: Normal and abnormal proximal esophageal acid exposure: Results of ambulatory Dual-probe pH monitoring. Am J Gastroenterol 88:25–29, 1993
Zaninotto G, DeMeester TR, Schwizer W, Johansson KE, Cheng SH: The lower esophageal sphincter in health and disease. Am J Surg 155:104–111, 1988
Stein HJ, DeMeester TR, Naspetti R, Jamieson J, Perry RE: Three-dimensional imaging of the lower esophageal sphincter in gastroesophageal reflux disease. Ann Surg 214:374–384, 1991
Crookes PF, Stein HJ, DeMeester TR: Stationary manometry of the esophageal body and upper esophageal sphincter. Probl Gen Surg 9:39–61, 1992
DeMeester TR, Wang CL, Wernly JA, Pellegrini CA, Little AG, Klementschitsch P, Bermudez G, Johnson LF, Skinner DB: Technique, indications and clinical use of 24-hour esophageal pH monitoring. J Thorac Cardiovasc Surg 79:656–670, 1980
Bremner RM, Constantini M, DeMeester TR, Bremner CG, Hoeft SF, Crookes PF, Peters JH, Hagen JA: Normal esophageal body function: A study using ambulatory esophageal manometry. Am J Gastroenterol 93:183–187, 1998
Anderson LI, Madsen PV, Dalgaard P, Jensen G: Validity of clinical symptoms in benign esophageal disease, assessed by questionnaire. Acta Med Scand 221:171–177, 1987
Bennett JR, Castell DO: Overview and symptom assessment. In The Esophagus. DO Castell (ed). Philadelphia, Lippincott Williams & Wilkins; 1999; pp 33–43
Constantini M, Crookes PF, Bremner RM, Hoeft SF, Ehsan A, Peters JH, Bremner CG, DeMeester TR: Value of physyological assessment of foregut symptoms in a surgical practice. Surgery 114:780–787, 1993
Schenk BE, Kuipers EJ, Klinkenber-Knol EC, Fasten HPM, Jansen EH, Tuynman HARE, Schrijver M, Dieleman LA, Meuwissen SGM: Omeprazole as a diagnostic tool in gastroesophageal reflux disease. Am Coll Gastroenterol 92:1997–2000, 1997
Caldarelli DD, Andrews AH, Derbyshire, AJ: Esophageal motility studies in globus sensation. Ann Otol Rhinol Laryngol 79:1098–1100, 1970
Mason RJ, Filipi CJ, DeMeester TR, Peters JH, Lund RJ, Flake AW, Hinder, RA, Smyrk TC, Bremner CG, Thompson S: A new intraluminal antigastroesophageal reflux procedure in baboons. Gastrointest Endosc 45:283–290, 1997
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tomonaga, T., Awad, Z.T., Filipi, C.J. et al. Symptom Predictability of Reflux-Induced Respiratory Disease. Dig Dis Sci 47, 9–14 (2002). https://doi.org/10.1023/A:1013290715062
Issue Date:
DOI: https://doi.org/10.1023/A:1013290715062