Abstract
Background
Community-acquired pneumonia (CAP) causes substantial clinical and economic burden. While several studies have reported the cost to treat CAP, there is little information on the cost to treat by age, risk profile, and hospitalization in US adults aged ≥50 years.
Objective
To quantify the cost, from a payer perspective, of treating CAP at the episode level, stratified by age, risk profile, and hospitalization.
Methods
A retrospective study of claims data from a large US health plan (1 January 2006–31 December 2008) was conducted. Patients aged ≥50 years having at least one medical claim with a primary diagnosis for pneumonia were identified. A CAP episode was defined as the period between the first and last pneumonia ICD-9 code with a chest X-ray claim. Episode-level variables included risk stratum based on presence of an immunocompromising/chronic condition, age group, number and length of inpatient and outpatient CAP episodes, and all-cause and CAP-related healthcare costs (adjusted to 2011 costs).
Results
Among the 27,659 study patients, 28,575 CAP episodes (20,454 outpatient; 8,121 inpatient) occurred. Mean age of patients with a CAP episode was 62.6. Low-risk patients accounted for 44.4 % of all CAP episodes. Mean CAP episode length was 31.8 days for an inpatient episode and 10.2 days for an outpatient episode. Mean all-cause total healthcare cost for an inpatient CAP episode ranged from $11,148 to $51,219 depending on risk stratum and age group. Mean outpatient episode-related costs were much lower than inpatient episode-related costs.
Conclusions
Cost to treat CAP requiring hospitalization is high regardless of age or the presence of underlying comorbidities. Given that almost half of the patients in this study did not have traditional risk factors for CAP, it is clear that better preventative strategies are needed.
Similar content being viewed by others
• The cost of treating CAP requiring hospitalization is high regardless of the presence of underlying comorbidities or age, although the cost rises substantially with increasing level of risk.
• Despite trends toward greater use of outpatient versus inpatient treatment, over a quarter of the commercially insured CAP patients aged ≥50 years in this study population were treated in a hospital setting.
• Even for low-risk patients in the 50- to 64-year age group, hospitalization was quite costly, with a mean cost of $15,385 (median $9,380).
1 Background
Community-acquired pneumonia (CAP) is an acute infection with potentially severe consequences, is associated with high hospitalization and mortality rates, and results in considerable economic burden [1]. In the US, approximately 5.6 million cases of CAP occur each year with circa one-quarter of those cases requiring hospitalization [2]. Roughly 1.3 million people in the US are admitted to the hospital with CAP annually, and re-admission rates within the first 30 days range from <1 to 20 % [3]. Among patients hospitalized for pneumonia, approximately 10–20 % are admitted to an intensive care unit [4, 5]. CAP is the sixth most common cause of death [1], with a case-fatality rate of up to 16 % for hospitalized CAP patients [6] and an overall 30-day mortality rate ranging from 1 to 23 % [1].
Risk factors for CAP include advanced age and comorbidities; these factors also increase the risk of adverse outcomes for those diagnosed with CAP [3, 7, 8, 9, 10, 11]. In the older adult population, increasing age is associated with an increase in CAP incidence [12, 13], hospitalizations [13], and mortality [12, 13]. Among the approximately 1.1 million people hospitalized for pneumonia (including CAP) in 2007, 21 % were aged 45–64 years, and 58 % were 65 or older [14]. To reduce the risk for CAP, the Infectious Diseases Society of America (IDSA) and the American Thoracic Society (ATS) consensus guidelines recommend that persons aged 50 years and over receive a yearly vaccination with the inactivated influenza virus and that persons aged 65 years and older receive a pneumococcal vaccination [15].
In the US, the direct cost of CAP is reported to be in excess of $17 billion annually [1]. However, the exact figure is unknown and likely to be underestimated as the CAP cost burden in the Medicare population alone was at least $13 billion in 2008 [16]. A separate study reported the annual burden of CAP to be $10.6 billion in working-age adults in 2010 [17]. To provide context, $2.6 trillion was spent on healthcare in the US in 2010 [18]. Estimated direct costs for a single CAP-attributable outpatient visit ranging from $130 to $4,500 were reported between the years 2000 and 2008 [19, 20, 21], conferring an annual cost of $9.3 billion (assuming 4 million outpatient CAP cases per year) [1, 20].
Although several studies have quantified the cost to treat CAP, few have evaluated the cost to treat by age, risk profile, and hospitalization in US adults. To address this gap in the literature, the present study evaluated the economic burden of CAP at the episode level in a sample of commercially insured patients aged ≥50 years with CAP, stratified by age, risk level, and inpatient versus outpatient episode. The study was limited to patients aged 50 years and older because of their higher risks for CAP [3, 7, 8, 9, 10, 11], the presence of increased comorbidities in this population [8, 9], and the prevention strategies outlined by the IDSA/ATS guidelines [15].
2 Methods
A retrospective study was conducted using integrated administrative medical and pharmacy claims data from the Optum Research Database, a large, proprietary US health insurance database affiliated with Optum. At the time of this study (2006–2007), approximately 13 million geographically diverse individuals with commercial medical and pharmacy benefit coverage, and 8.6 million with medical coverage only, were enrolled in this geographically diverse, commercially insured, national managed care health plan. The health plan provides fully insured coverage for professional, facility, and outpatient prescription medication services.
2.1 CAP Episode Identification
Patients with at least one medical claim with a primary diagnosis of pneumonia were identified between 1 July 2006 and 31 December 2007. Pneumonia was identified based on International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes of 480, 481, 482.xx-483.xx, 484.xx, 485, 486, and 487.0 from an outpatient or inpatient venue. These codes have been used in previously published studies to identify CAP [10, 14, 22, 23]. The service date of the first observed pneumonia claim was defined as the index date. Patient inclusion criteria were a chest X-ray claim within 14 days of the index date (to distinguish CAP from other respiratory conditions), aged 50 years or older, and continuous enrollment with full benefits for at least 90 days prior to the start of the episode. To refine CAP identification, patients were excluded if they resided in a nursing home or other long-term care facility in the 14 days prior to the index date or if they were hospitalized for any reason in the 14 days before the index date. Demographic and clinical characteristics of patients with CAP episodes were assessed during the pre-index period.
A CAP episode length was defined as the period between the first medical claim with a primary diagnosis for pneumonia (index date) and the last medical claim for pneumonia in the primary or secondary position. The cutoff for an episode start date was 15 December 2007 to allow for at least 2 weeks of observation. Episodes that ended beyond the date for which 90 days could be observed between the last pneumonia medical claim and 31 December 2007 were censored at 31 December 2007. Additionally, patients were required to have a 90-day period free of pneumonia claims before and after the CAP episode (clean-period), unless they died during the CAP episode (as determined from the LexisNexis® “Accurint” database, which accesses Social Security Administration death tapes) to distinguish one episode from another in the same person and to “close” the episode period.
2.2 Healthcare Costs
All-cause total healthcare costs and CAP-related healthcare costs [pharmacy, office visits, ambulatory visits, emergency room (ER) visits, inpatient visits, and other costs] were calculated by combining health plan and patient-paid amounts incurred during each CAP episode. All-cause costs were considered because CAP can exacerbate an underlying medical condition, which may result in additional costs. CAP-related healthcare costs were also computed based on medical claims of pneumonia in the primary or secondary diagnosis position and any pharmacy claims for antibiotics occurring within 2 days of a medical claim for pneumonia. For an inpatient stay with a primary or secondary pneumonia diagnosis, all the costs for the particular hospital stay were attributed as CAP-related costs. These data provide a good estimation of total costs of care from a payer perspective, which is a key consideration as payer-negotiated allowable amounts with providers include combined health plan and patient-paid amounts. The study focused on the costs of the episode as a whole and not a cost comparison of individual procedures and treatments. Costs were adjusted using the annual medical care component of the Consumer Price Index (CPI) to reflect inflation between 2007 and 2011 [24].
2.3 Stratification Variables
Because underlying factors such as age, comorbidity, and setting of care lead to variation in the costs of treating CAP, the data were stratified by these three variables. The risk of developing CAP (low, moderate, high) was defined based on the presence of immunocompromising or chronic conditions [25, 26] at any time during the pre-episode clean period through the end of the post-episode clean period. High-risk patients had at least two claims falling within the same condition, on separate dates, indicating a particular immunocompromising condition [see Appendix A (electronic supplementary material) for relevant diagnosis/procedure codes and Appendix B (electronic supplementary material) for relevant medications]. Patients were considered to be at moderate risk if they were immunocompetent and had at least two medical claims falling within the same condition, at least 30 days apart, with primary diagnoses for a particular chronic condition [codes shown in Appendix C (electronic supplementary material)]. Patients not classified as moderate or high risk were considered to be at low risk.
A CAP inpatient episode was defined as at least one pneumonia-related (primary or secondary diagnosis) inpatient stay; episodes not identified as inpatient were deemed to be outpatient episodes. Age was stratified according to the following: 50–64, 65–74, 75–84, and ≥85 years old.
2.4 Analyses
All study variables were analyzed descriptively and conducted at an episode level. In addition to costs, other factors examined include episode length, length of hospital stay including re-hospitalization for inpatient episode, and cost components. Analyses were stratified by age, the setting of care, and risk stratum.
3 Results
3.1 Patient Demographic and Clinical Characteristics
After applying all inclusion and exclusion criteria, there were 27,659 patients who experienced 28,575 CAP episodes (Fig. 1). The vast majority of patients (97 %) had only one episode during the CAP identification period.
Of the 28,575 CAP episodes, 28 % were treated in an inpatient setting and 72 % were treated in an outpatient setting. Across both treatment settings, the mean age of patients with a CAP episode was 62.6 [SD 10.1] years, with both genders represented equally (Table 1). Among the inpatient CAP episodes, chronic obstructive pulmonary disease was the most common (36 %) chronic condition represented; among outpatient CAP episodes, diabetes was the most prevalent chronic condition (15.3 %). Across both treatment settings, 44.4 % of the total episodes occurred in patients categorized as low-risk who did not have traditional risk factors for CAP; however, the proportion of CAP episodes occurring in low-risk patients varied by treatment setting, with 55.0 % of the outpatient CAP episodes and only 17.7 % of inpatient episodes occurring in low-risk patients.
3.2 Length of CAP Episode and Inpatient Stay
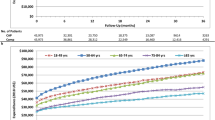
Overall, the mean CAP episode length was 31.8 [SD 47.6] days for an inpatient episode and 10.2 [SD 23.7] days for an outpatient episode (Fig. 2). In general, the episode length increased with increasing age, reaching approximately 35 and 14 days for inpatient and outpatient episodes, respectively, for patients aged ≥75 years. The episode length also increased with higher risk. For inpatient episodes among patients aged ≥50 years, the mean [SD] episode length was 24.7 [30.4], 30.5 [46.6], and 39.5 [57.3] days for the low-, moderate-, and high-risk groups, respectively. The median episode length was much lower: 14 days for an inpatient episode and 1 day for an outpatient episode. This suggests that over half of the outpatient episodes involved only one healthcare encounter.
Overall, the mean number of inpatient stays for a CAP episode was 1.09 for patients ≥50 years of age. The overall mean length of stay, which may have included any re-hospitalization during the CAP episode, was 7.1 days. The length of stay increased with increasing levels of risk, with a mean of 4.8, 6.8, and 9.5 days for the low-, moderate-, and high-risk groups, respectively, for patients aged ≥50 years.
3.3 All-Cause Healthcare Costs
The overall mean cost for an outpatient episode was $2,212, but it was substantially higher for an inpatient episode ($27,661) (Fig. 3). For most age and risk groups, the cost of an outpatient episode was about one-tenth to one-eighth of the cost of an inpatient episode. As expected, the cost of an episode rose with increasing risk within an age group. However, even in the aged 50–64 years low-risk group, the mean cost to treat CAP in a hospital setting was high at $15,385 (Table 2). The median cost was much lower ($9,380), suggesting a skewed cost distribution. For both outpatient and inpatient CAP episodes, there was a wider range of mean costs across risk strata than across age groups.
For outpatient episodes, the majority of costs were due to ambulatory visits and other medical costs, which include non-pneumonia-related inpatient costs (Fig. 3). Pharmacy costs comprised only 9.7 % of outpatient episode costs. For inpatient episodes, 85.1 % of the all-cause costs were due to inpatient care.
3.4 CAP-Related Healthcare Costs
CAP-related healthcare costs represented 93.2, 90.0, and 81.4 % of the all-cause total healthcare costs for inpatient episodes for low-, moderate-, and high-risk patients aged ≥50 years, respectively. For outpatient episodes, CAP-related costs represented 55.7, 41.2, and 28.3 % of all-cause total healthcare costs incurred by low-, moderate-, and high-risk patients, respectively.
4 Discussion
CAP is a common respiratory illness and is a frequent cause of hospitalization. In our study population of patients aged ≥50 years, about 28 % of the CAP episodes required an inpatient hospitalization. Low-risk patients had the highest proportion of patients with an outpatient episode among patients aged 50 years and over, and high-risk patients had the highest proportion of patients with an inpatient episode. The mean length of hospital stay increased with age and risk level. Although the length of stay was almost twice as long for the oldest age group compared with the 50- to 64-year age group, a mean stay of 4.8 days constitutes a longer inpatient hospitalization than one might expect with a relatively healthy younger age group. In general, the older age groups have greater comorbidity, so inpatient CAP-related stays would be expected to be longer when underlying conditions are being managed as well.
The mean numbers of inpatient days we observed are in line with those cited in recent studies, which have reported mean lengths of stay ranging from 4 to 12 days among patients with CAP [3, 5, 27]. However, our mean lengths of stay were longer than the national average reported in the National Hospital Discharge Survey, where the average length of stay for pneumonia discharges was 5.1 days in patients aged 45–64 years and 5.4 days in patients aged ≥65 years [14, 28]. We attribute the longer inpatient stays in our study to the fact that our overall length of stay included hospital days spent caring for pneumonia, non-pneumonia-related complications or comorbidities, and any re-hospitalization required within the same inpatient CAP episode.
Patients who had an inpatient episode incurred high all-cause and CAP-related total healthcare costs regardless of age or risk stratum. The all-cause cost of an outpatient episode was only a small fraction (8 %) of that of an inpatient episode, whereas inpatient stay was the predominant cost component for an inpatient episode, comprising 85.1 % of the total cost. All-cause total healthcare costs incurred by patients in the 50- to 64-year age group were similar to those incurred by older patients such as those in the 75- to 84-year age group. Even for low-risk patients in the 50- to 64-year age group, hospitalization was quite costly, with a mean cost of $15,385 (median $9,380).
The proportion of CAP-related costs decreased with increasing risk stratum. This suggests that a greater proportion of healthcare dollars was spent to treat underlying conditions in higher risk patients than in low-risk patients. Consistent with previously published results, we found that CAP represents a substantial economic burden, particularly when hospitalization becomes necessary [1, 20, 21]. Our study is unique, however, in that we have stratified CAP episode-level cost data by age and risk stratum. Stratifying the analysis by risk level, based on the presence of an immunocompromising or chronic condition, enabled us to examine the impact of comorbidities on costs. The mean incremental cost increase with each increasing risk stratum was at least several thousand dollars for an inpatient episode. While there was also variability in cost by age, that range of costs was much narrower than the range observed across risk groups, suggesting that comorbidities have greater impact than age in determining cost outcomes for CAP.
4.1 Study Limitations
The limitations on the use of administrative claims data for cost-of-illness studies are well recognized. Claims data are collected for the purpose of payment and not research, and are subject to possible coding errors, undercoding, and coding for the purpose of ruling out a suspected disease rather than determining the actual disease. Some of the outpatient episodes could have been misclassified as pneumonia when in fact they may have been respiratory-related episodes, as half of the identified CAP patients had an episode of only 1 day. However, it is clinically feasible for mild CAP cases to have only one outpatient healthcare encounter. Due to the robust sample size, small misclassifications are unlikely to have substantially altered results. While we did not validate the case definition of CAP in this study, we used pneumonia codes from similar previous studies [10, 14, 22, 23] and applied additional criteria to better identify CAP.
The definition of length of episode duration used in this study may have resulted in longer illness duration than what is typically observed in clinical practice and therefore may have resulted in overestimation of costs. Although there is evidence to support the fact that CAP symptoms linger well beyond the period of antibiotic prescription [29], we captured episode duration by economic resource use based on pneumonia-related claims, rather than from a strict clinical perspective.
Our study population was a sample of managed care enrollees; therefore, results may not be generalizable to other populations. Finally, the data used for this study pertain to costs of CAP episodes incurred in 2007 and therefore may not accurately represent current cost patterns. However, we CPI-adjusted episode level costs to 2011 dollars.
Despite these limitations, administrative data allow for examination of healthcare utilization and expenditure patterns in a real-world setting and offer the advantage of large sample sizes with diverse medical histories.
5 Conclusions
Hospitalization is the most costly factor in the management of CAP. Despite trends toward greater use of outpatient versus inpatient treatment, over a quarter of these commercially insured CAP patients aged ≥50 years were treated in a hospital setting. Cost to treat CAP requiring hospitalization is high regardless of the presence of underlying comorbidities or age, although the cost rises substantially with increasing level of risk. Given that almost half (44 %) of the CAP patients in this study did not have traditional risk factors for CAP, it is clear that efforts to better implement preventative strategies as recommended by IDSA/ATS CAP management guidelines [15]—i.e., vaccination targeting influenza and pneumococcal disease for older adults and for individuals with medical conditions that place them at high risk for pneumonia morbidity and mortality—are needed to reduce the incidence and economic burden of CAP.
References
File TM Jr, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122:130–41.
Brar NK, Niederman MS. Management of community-acquired pneumonia: a review and update. Ther Adv Respir Dis. 2011;5:61–78.
Metersky ML, Ma A, Houck PM, et al. Antibiotics for bacteremic pneumonia: improved outcomes with macrolides but not fluoroquinolones. Chest. 2007;131:466–73.
Marrie TJ, Shariatzadeh MR. Community-acquired pneumonia requiring admission to an intensive care unit: a descriptive study. Medicine (Baltimore). 2007;86:103–11.
Restrepo MI, Mortensen EM, Velez JA, et al. A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest. 2008;133:610–7.
Colice GL, Morley MA, Asche C, et al. Treatment costs of community-acquired pneumonia in an employed population. Chest. 2004;125:2140–5.
Marrie TJ, Huang JQ. Low-risk patients admitted with community-acquired pneumonia. Am J Med. 2005;118:1357–63.
McAlister FA, Majundar SR, Blitz S, et al. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28:810–5.
Ewig S, Woodhead M, Torres A. Towards a sensible comprehension of severe community-acquired pneumonia. Intensive Care Med. 2011;37:214–23.
Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39:1642–50.
Ramsdell J, Narsavage GL, Fink JB. Management of community-acquired pneumonia in the home. An American College of Chest Physicians Clinical Position Statement. Chest. 2005;127:1752–63.
Conte HA, Chen Y-T, Mehal W, et al. A prognostic rule for elderly patients admitted with community-acquired pneumonia. Am J Med. 1999;106:20–8.
Stupka JE, Mortensen EM, Anzueto A, et al. Community-acquired pneumonia in elderly patients. Aging Health. 2009;5:763–4.
Hall MJ, DeFrances CJ, Williams SN, et al. National Hospital Discharge survey: 2007 summary. National Health Statistics Report Hyattsville, MD: National Center for Health Statistics; 2010. p. 1–21.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44:S27–72.
Yu H, Rubin J, Dunning S, Li S, Sato R. Clinical and economic burden of community acquired pneumonia in the Medicare fee-for-service population. J Am Geriatr Soc. 2012;60:2137–43.
Bonafede MM, Suava JA, Wilson KL, Mannino DM, Polsky D. Incidence and cost of CAP in a large working-age population. Am J Manag Care. 2012;18:380–7.
Martin AB, Lassman D, Washington B, Catlin A, the National Healthcare Expenditure Accounts Team. Growth in US health spending remained slow in 2010; health share of gross domestic product was unchanged from 2009. Health Aff. 2012;31:1208–19.
Restrepo MI, Frei CR. Health economics of use of fluoroquinolones to treat patients with community-acquired pneumonia. Am J Med. 2010;123:S39–48.
Sun HK, Nicolau DP, Kuti JL. Resource utilization of adults admitted to a large urban hospital with community-acquired pneumonia caused by Streptococcus pneumoniae. Chest. 2006;130:807–14.
Orrick JJ, Segal R, Johns TE, et al. Resource use and cost of care for patients hospitalized with community-acquired pneumonia: impact of adherence to Infectious Diseases Society of American guidelines. Pharmacoeconomics. 2004;22:751–7.
Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;137:552–7.
Lindenauer PK, Bernheim SM, Grady NJ, et al. The performance of US hospitals as reflected in risk-standardized 30-day mortality and readmission rates for Medicare beneficiaries with pneumonia. J Hosp Med. 2010;5:E13–8.
US Department of Labor. Consumer Price Index. Chained Consumer Price Index for all urban consumers (C-CPI-U) 1999–2008. Medical Care Series ID: SUUR0000SAM. Washington, DC: U.S. Dept. of Labor, Bureau of Labor Statistics; 2008.
Centers for Disease Control and Prevention. Prevention of pneumococcal disease: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR. 1997;46:1–24.
Centers for Disease Control and Prevention (CDC), Advisory Committee on Immunization Practices. Updated recommendations for prevention of invasive pneumococcal disease among adults using the 23-valent pneumococcal polysaccharide vaccine (PPSV23). MMWR Morb Mortal Wkly Rep. 2010;59:1102–6.
Kaplan V, Angus DC, Griffin M, et al. Hospitalized community-acquired pneumonia in the elderly: age- and sex-related patterns of care and outcome in the United States. Am J Respir Crit Care Med. 2002;165:766–72.
DeFrances CJ, Lucas CA, Bule VC, et al. 2006 National Hospital Discharge Survey. Natl Health Stat Rep. 2008;30:1–20.
Metlay JP, Fine MJ, Schulz R, et al. Measuring symptomatic and functional recovery in patients with community-acquired pneumonia. J Gen Intern Med. 1997;12:423–30.
Acknowledgments
The study described in this article was sponsored by Wyeth, which was acquired by Pfizer, Inc., in October 2009. The study sponsor played a significant role in the analysis and interpretation of data, the writing of the article, and the decision to submit it for publication. Optum was hired by Pfizer, Inc., to collect the data and conduct the analyses for this study. Reiko Sato conceived the study question. Gabriel Gomez Rey, Stephanie Nelson, and Brett Pinsky were involved in the data collection for this study. All authors made significant contributions to the design of the study, the data analysis, and manuscript preparation. The final version submitted for publication was approved by all authors. Brett Pinsky takes responsibility for the content of the manuscript. The authors thank Victoria Porter (BA; medical writer) and Laura Oberthur Johnson (PhD, medical writer), employees of Optum, for their assistance with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited. The exclusive right to any commercial use of the article is with Springer.
About this article
Cite this article
Sato, R., Gomez Rey, G., Nelson, S. et al. Community-Acquired Pneumonia Episode Costs by Age and Risk in Commercially Insured US Adults Aged ≥50 Years. Appl Health Econ Health Policy 11, 251–258 (2013). https://doi.org/10.1007/s40258-013-0026-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-013-0026-0