Abstract
A majority of congenital heart defects are due to abnormal development of the valves and membranous septa, i.e., connective tissue components of the heart. During development, an interesting feature of cardiac connective tissue is transient expression of collagens typical for cartilage. To better understand the role of these collagens in the heart, we have performed a systematic study on the temporospatial expression of type II and IX collagen isoforms during mouse heart development employing northern hybridization and RNase protection assay. The mRNAs for α1(II) and α1(IX) collagens were expressed transiently between embryonic days 10.5 and 14.5 in embryonic mouse heart. RNase protection assays revealed that for both transcripts the embryonic ("prechondrogenic") variants of the alternatively spliced mRNA isoforms dominated. Immunohistochemistry demonstrated that type IIA collagen and Sox9, its key transcriptional regulator, were expressed in the epithelial–mesenchymal areas of the developing heart, with partially overlapping patterns particularly in valvular and septal regions. In addition, Sox9 expression was detected widely in the developing heart. These observations support the hypothesis that cartilage collagens, especially the long isoform of type II collagen, participate in the morphogenesis of cardiac valves and septa.
Similar content being viewed by others
Introduction
Several lines of evidence suggest that extracellular matrix (ECM) plays an important role in the complex process of heart development. During early cardiac development, ECM is involved in migration of endocardial cells to the atrioventricular area and in their epithelial–mesenchymal transformation (Borg et al. 1990; Markwald et al. 1996). ECM molecules are also involved in the binding of growth factors and other molecules, which further regulate cell differentiation and migration (Borg et al. 1990; Little and Rongish 1995; Lamers and Moorman 2002). Cardiac valves and septa are also derived from ECM of endocardial cushion (Little and Rongish 1995, Lamers and Moorman 2002). ECM provides the heart with stress tolerance against forces generated during the cardiac cycle in the developing heart (Nakagawa et al. 1992; Carver et al. 1993). As collagens form the main component of cardiac ECM, their role in myocardial development and heart function is likely to be a dominant one (Borg et al. 1990). Out of the 20 known collagen types 3 fibril-forming collagens (types I, III, and V) form heterotypic fibrils, the main component of the connective tissue network in the adult heart (Bishop and Laurent 1995), the valves, and the large vessels (Little and Rongish 1995).
An interesting feature of ECM in the developing heart is transient expression of type II, IX, and XI collagens, which have traditionally been considered to be specific for cartilage (Mendler et al. 1989). Transcripts of α1(II) collagen have been detected in embryonic chick and fetal human hearts (Nah and Upholt 1991; Sandberg et al. 1993; Swiderski et al. 1994) and in E9.5–E10.5 mouse hearts (Cheah et al. 1991; Ng et al. 1993). During embryonic development, expression of type IX collagen mRNA has also been observed in the mouse heart (Liu et al. 1993). Low level expression of cartilage collagens has been observed in some other developing non-cartilaginous tissues, too (Thorogood et al. 1986; Kosher and Solursh 1989; Wood et al. 1991; Burgeson and Nimni 1992; Sandberg et al. 1993).
A characteristic feature of type II and IX cartilage collagen transcripts is their developmental and tissue specific alternative splicing. Type II collagen, a homotrimer of α1(II) chains, is the major fibrillar collagen in cartilage. The long isoform (type IIA) predominates during embryogenesis, whereas the short isoform (type IIB) is characteristic to mature cartilage (Ng et al. 1993; Lui et al. 1995; Oxford et al. 1995). Type IX collagen, a heterotrimer of α1(IX), α2(IX), and α3(IX) chains is attached on the surface of cartilage collagen fibrils (Smith and Brandt 1992). The gene coding for the α1(IX) chain has two promoters which results in long and short mRNA and protein isoforms (Liu et al. 1993). The long isoform is characteristic of mature cartilage, and the short one of prechondrogenic mesenchyme and non-cartilaginous tissues (Brewton et al. 1991; Perälä et al. 1997).
To better understand the role of type II and IX cartilage collagens in cardiac development we decided to perform a systematic study on the temporospatial expression of these collagens in the mouse heart with special emphasis on embryonic stages E10.5–E12.5, which are the critical time points in the development of valves and septa (Webb et al. 1998). As transcription factor Sox9 has been shown to be required for cartilage differentiation and the expression of type II and XI collagen genes (Bridgewater et al. 1998; de Crombrugghe et al. 2000), we also analyzed the expression of Sox9 in the mouse heart during cardiogenesis.
Materials and methods
RNA extraction and northern analysis
Total RNA was isolated from dissected (n=3 at each time point) hearts of normal (NMRI white) mice at daily intervals between embryonic days 10.5–18.5 (marked E10.5–E18.5), and of adult mice, as well as from cartilages of E17.5 mice, by homogenization in 4 mol/l guanidine isothiocyanate followed by sedimentation through 5.7 mol/l cesium chloride (Chirgwin et al. 1979). Alternatively, an RNAzol b kit (Tel Test, Houston, TX, USA) was used as recommended by the manufacturer. The study protocol was approved by the institutional committee for animal welfare.
For northern analysis, 10 μg aliquots of total RNA were run on 1% agarose gels and the samples were transferred onto Pall Biodyne membranes overnight by blotting, as recommended by the supplier (Pall Europe, Portsmouth, UK). For hybridizations, purified inserts were labeled by random priming to specific activities of approximately 1×109 with 32P-dCTP. The mRNAs for proα1(II), α1(IX), α2(IX), α3(IX), and α1(XI) collagens were detected using cDNA clones pMCol2a1-1 (Metsäranta et al. 1991), pMCol9a1-1 (Metsäranta et al. 1991), pMCol9a2-1 (Elima et al. 1992), pMCol9a3-1 (Perälä et al. 1997), pMCol10a1-1 (Elima et al. 1992), pMCol11a1-1 (Perälä et al. 1997), and pM28S (Joronen et al. 2000). The hybridizations were performed at 42°C in 50% formamide, 1 mol/l NaCl, 1% sodium dodecyl sulfate (SDS), 10% dextran sulfate, 5×Denhardt's solution, and 100 μg/ml sonicated calf thymus DNA, and the high stringency washes at 55°C in 0.1×SSC, 0.1% SDS. After washes the filters were analyzed and quantified using the Molecular Imager phosphoimager (BioRad, Hercules, CA, USA).
In situ hybridization
Details of the technique used have been described earlier (Sandberg and Vuorio 1987; Ylä-Herttuala et al. 1990). Briefly, the tissue samples were fixed with 4% paraformaldehyde overnight and embedded in paraffin for sectioning. Longitudinal and sagittal sections of mouse embryos and newborn mice were cut onto organosilanated slides. For in situ hybridization, the sections were pretreated with proteinase K (5 μg/ml for 30 min at 37°C) and acetylated. The hybridizations were performed at 53–55°C for 18–24 h. Antisense and sense riboprobes were synthesized using a Trans-Probe-T kit (Pharmacia, Uppsala, Sweden) and 35S-(thio)UTP (>1,000 Ci/mmol; Amersham International, Amersham, UK), and an extended incubation time of 1.5 h for transcription. After digestion with DNase I, the reactions were incubated at 65°C for 15 min, cooled on ice, and fractionated on a Sephadex G-50 column (Pharmacia). Hybridization was followed by washes in SSC-EDTA and in phosphate-buffered saline (PBS) and autoradiography for 7–35 days and counterstaining of sections with hematoxylin.
RNase protection assay
The ratios of the long and short isoforms of proα1(II) and proα1(IX) collagen mRNAs were studied by RNase protection assay as described earlier (Savontaus et al. 1997). The proα1(II) collagen transcripts were determined using clone pMCol2a1-(2→7), which contains a 465-bp insert covering the sequence from the middle of exon 2 (nucleotide 105) to the end of exon 7 (Savontaus et al. 1997). The α1(IX) collagen mRNA isoforms were analyzed using clone pMCol9a1-3, containing a 78-bp insert specific for the short form and a 124-bp fragment specific for the long form of the mRNA (Savontaus et al. 1998).Solution hybridization was performed at 55°C using 5×105 cpm of probe and 10 μg of total RNA. After hybridization, the samples were digested with RNase A and T1, and proteinase K, and precipitated for electrophoresis on denaturing 4.5% (type II collagen) or 6.0% (type IX collagen) gels with end-labeled fragments of plasmid pBR322 digested with MspI as standards. After fixation and drying, the gels were exposed on X-ray films and quantified on a phosphoimager.
Immunohistochemistry
Cardiac distribution of type II collagen was studied using a monoclonal antibody against chick type II collagen (Linsenmayer and Hendrix 1980). The long isoform of type IIA procollagen was studied using rabbit polyclonal antiserum raised against mouse recombinant type IIA procollagen peptide (Salminen et al. 2001; Säämänen et al. unpublished results). The distribution of Sox9 was studied using polyclonal antibodies against human Sox9 (Mertin et al. 1999). Tissue sections were deparaffinized, rehydrated, and digested at 37°C for 1 h with hyaluronidase (2 mg/ml) in PBS (pH 5). After washing, the type II collagen primary antibody (1:100 dilution) or type IIA (1:200 dilution) antibody or Sox9 (1:500 dilution) antibody was applied and incubated overnight at +4°C. The sections were washed and incubated consecutively with biotin-labeled secondary antibody. The secondary antibodies were detected using the avidin-biotin method (Histostain-Plus kit; Zymed, South San Francisco, CA, USA) as above. Color was developed with diaminobenzidine (DAB-Plus kit; Zymed), and the sections were counterstained with hematoxylin. For control staining, preimmune serum was used instead of the primary antibody.
Results
Developmental expression of type II, IX, and XI collagen mRNAs in the mouse heart
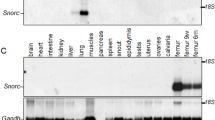
The expression of type II collagen mRNA in the developing mouse heart was at its highest level already at E10.5 (Fig. 1A). Thereafter the expression gradually declined and no expression was seen after E14.5–E15.5 (Fig. 1A). The α1(IX) collagen mRNA exhibited a similar temporal expression pattern (Fig. 1B). However, no expression of α2(IX) and α3(IX) collagen mRNAs could be detected by northern analysis at any stage of heart development. Unlike the transient expression of type II and α1(IX) collagen mRNAs, low levels of α1(XI) collagen transcripts were detectable in the heart through embryogenesis without any marked change in the expression level (Fig. 1C).
Northern analysis of total RNAs (10 μg) isolated from stage E10.5–E18.5 embryonic mouse hearts, from adult mouse heart, and from E17.5 sternal cartilage, serving as a positive control (shown above the lanes). The hybridizations were performed with cDNA probes detecting both forms of proα1(II) collagen mRNA (A), both forms of α1(IX) collagen mRNA (B), proα1(XI) collagen mRNA (C), and 28S rRNA (D)
RNase protection assay
Simultaneous analysis of the two alternative isoforms of type II and IX collagen mRNAs by RNase protection assays confirmed that both type IIA and IIB collagen mRNA isoforms and the short isoform of α1(IX) collagen mRNA were at their highest level in E10.5 hearts (Fig. 2). No α1(II) collagen mRNA was seen after stage E15.5. Unlike cartilage, the embryonic heart exhibited both isoforms of type II collagen with the type IIA isoform predominating (Fig. 2). As in the developing eye (Savontaus et al. 1997), the short isoform of α1(IX) mRNA was seen transiently in the developing heart during E10.5–E12.5 (Fig. 2).
Determination of the different isoforms of the proα1(II) and α1(IX) collagen mRNAs during heart development by RNase protection assay. Total RNA (10 μg) isolated from stage E10.5, E11.5, E12.5, E13.5, E15.5, and E17.5 embryonic mouse hearts, adult mouse heart, and E17.5 sternum (shown above the lanes) was hybridized with cRNA probes specific for A the proα1(II) collagen mRNAs (the sizes of protected fragments are 465 bp for type IIA and 365 bp for type IIB collagen) and B α1(IX) collagen mRNAs (the sizes of protected fragments are 124 bp for the long isoform and 78 bp for the short one). Protected fragments were subjected to electrophoresis with end-labeled MspI fragments of pBR322 as standards. Undigested probes were run on the left, and probes hybridized with yeast tRNA on the right
Localization of α1(II) collagen mRNA by in situ hybridization
No expression of either α1(II) or α1(IX) mRNA was detected at E9.5 by in situ hybridization. The appearance of α1(II) collagen mRNA was transiently detected only at E10.5–E11.5 with diffuse expression in the ventricular and atrial walls (Fig. 3). No clear signal between background levels of α1(IX) collagen transcripts were detected in stage E10.5 hearts (data not shown).
Localization of proα1(II) collagen mRNA by in situ hybridization in mouse heart at 10.5 days of embryonic development. Diffuse hybridization signal in the walls of atria and ventricles with probe pMCol2a1-1 detecting both forms of proα1(II) collagen mRNAs is best seen in darkfield micrograms (B). The anatomical structures are indicated in the corresponding brightfield micrograph (A). a Atrium, v ventricle. Bar in A corresponds to 200 μm in panels A and B
Immunohistochemistry
Using a polyclonal antibody capable of detecting the long isoform of type II collagen, the positive immunoreactivity was localized at E9.5 in endothelial–mesenchymal interfaces of the ventricle wall of primary heart and in the atrioventricular canal region (Fig. 4). At E11.5 strong positive staining for type IIA collagen was seen in the endocardial cushion region and at a low level also in primitive trabeculae, which may develop into chordae tendiniae (Fig. 5). When monoclonal antibody capable of detecting both isoforms of type II collagen was used, the signal was weaker and more diffuse but located in the same areas as the positive staining for type IIA collagen was localized (Fig. 5). As the development proceeded to day E12.5 the positive immunostaining was detected in epithelial–mesenchymal interfaces of the septa, in the atrioventricular canal, the endocardial cushion between atria and ventricles, and the septum primum, as well as in the pericardium and the primitive chordae tendiniae of the developing heart (Fig. 6). Interestingly, at E12.5 the expression of type IIA collagen become highly localized in the epithelial–mesenchymal interfaces of septa and primitive trabeculae (Fig. 6B). Protein expression was transient as no type II or type IIA collagen was seen in the heart at E15.5 or later (data not shown). Serial sections were also studied using monoclonal antibodies to type II collagen capable of detecting both isoforms IIA and IIB. At all time points, only a weak signal could be identified. No differences were seen in the tissue distribution of total type II and type IIA collagen (a representative example is shown in Fig. 5).
Immunolocalization of type IIA collagen (A–C) and transcription factor Sox9 at E9.5. Positive staining of type IIA collagen is mainly seen in endothelial–mesenchymal interfaces of the ventricle wall of heart (arrowhead), and in the primitive valvular structures of the atrioventricular canal (arrows). Sox9 was localized widely in the wall of the primitive ventricle and atria and in the atrioventricular canal (D, E). No unspecific reactivity was seen in the negative control (F). Bar in A corresponds to 50 μm (for A, D, F), to 20 μm (for B, E), and to 12.5 μm (for C)
Immunolocalization of type II and IIA collagens and transcription factor Sox9 at E11.5. Immunoreactivity for type IIA collagen (A) was at a low level in trabeculae of myocardium, at the interface of pericardium and epicardium, and in the cardiac jelly with the strongest immunostaining in the endocardial cushion region (A–C arrowhead). For comparison, immunolocalization of both isoforms of type II collagen is shown in G and H. Immunodetection of Sox9 was more widespread in the nuclei of heart muscle cells (D, E). No staining was seen in the negative staining control (F). a Atrium, v ventricle, arrowhead endocardial cushion. Bar in A corresponds to 100 μm (for A, D, F, G), to 25 μm (for B, C, E), and to 12.5 μm (for H)
Immunohistochemical detection of type IIA collagen and transcription factor Sox9 at E12.5. Immunostaining for type IIA collagen was detected at the epithelial–mesenchymal interfaces of primitive trabeculae (A, C) and in septal structures (B). The boxed areas b and c are enlarged in panels B and C. Strong immunostaining was seen also in cartilaginous structures serving as positive controls. Sox9 was localized in the nuclei of some, but not all cardiac cells (D–F). The boxed areas e and f in panel D correspond to panels E and F. a Atrium, v ventricle. Bar in A corresponds to 100 μm (for A, D) and to 12.5 μm (for B, C, E, F)
Finally, immunohistochemistry revealed the expression of Sox9 in almost all compartments of the heart. (Figs. 4, 5, 6). Strong expression was detected in the nuclei of cardiac cells in the developing heart at stages E9.5–E13.5 (Figs. 4, 5, 6). The expression of Sox9 was also detected in cells located in the walls of ventricles and atria surrounded by type IIA collagen. Interestingly, nuclear Sox9 staining of cardiac cells started to disappear earlier than type IIA collagen staining in their matrix, as shown for E12.5 (Fig. 5). Furthermore, low levels of Sox9 were also detected at later stages of heart development (data not shown).
Discussion
Congenital malformations of the heart are the most common birth defects in humans. Abnormal development of cardiac valves and septa comprise most of such defects. In the present study we demonstrate that expression of proα1(II) and α1(IX) collagen genes in the mouse heart coincides with the formation of valvular and septal regions. Type IIA collagen gene was also expressed in early ventricular trabeculae. Both isoforms of the α1(II) collagen were expressed at comparable levels in the developing mouse heart. However, the long isoform (type IIA) was the dominating one and was focused in epithelial–mesenchymal interfaces of valvular and septal structures whereas the distribution of immunostaining with antibodies capable of detecting both isoforms of type II collagen was more homogenous. The latter stained several areas of the developing heart: developing chordae, endocardial cushions, membranous septa, and developing atrioventricular valves. Neither variant of type II collagen was seen in the heart after stage E14.5. These observations extend earlier studies on the localization of the corresponding mRNA in the embryonic heart (Thorogood et al. 1986; Kosher and Solursh 1989; Burgeson and Nimni 1992; Sandberg et al. 1993). In an earlier study (Wood et al. 1991), type II collagen was found in the interface between the epimyocardium and endocardium already at stage E9, but later time points were not studied.
Type IX collagen is generally coexpressed with type II collagen but at a lower level, with the short isoform of the α1(IX) chain being the dominant one in non-chondrogenic tissues (Liu et al. 1993), and the long one in mature cartilage. In the present study, RNase protection assay revealed that the short isoform of α1(IX) collagen mRNA also predominates during mouse cardiogenesis. As no mRNA for the α2 or α3 chains of type IX collagen was seen at any stage of cardiac development by using RT-PCR (data not shown), no normal heterotrimeric type IX collagen can be produced. Although α1(IX) chains have been shown to form trimers in vivo, no functional homotrimeric protein has been identified in vitro (Pihlajamaa et al. 1999). Consequently, the function of α1(IX) collagen mRNA in developing heart remains unclear and was not studied further in the present report.
Transient production of type II collagen and α1(IX) collagen mRNA in the developing heart remains without a generally accepted biologic explanation. One possibility is that cartilage collagen fibrils serve an instructive role for the correct formation of the three-dimensional network of major collagens (type I and III) in the heart. This would be analogous to the replacement of cartilaginous anlagen by bone during endochondral ossification (Uusitalo et al. 2001). The instructive role hypothesis is supported by observations of shortened heart valves in transgenic mice with targeted inactivation of the type II collagen gene (Li et al. 1995). Hypochondrogenesis, a chondrodysplasia caused by mutations in the type II collagen gene, has also been associated with congenital heart defects (Potocki et al. 1995). In the present study, we demonstrate that the type II collagen which is transiently expressed in cardiac valves, septa, and early trabeculae of the ventricles is of type IIA. As the expression coincides with the developmental stages critical for the specification of these structures, it is likely that type IIA collagen plays a role in these processes. This interpretation is supported by a recent preliminary report on severe cardiac malformations in transgenic mice harboring Col2a1 genes without exon 2 sequence (Cheah et al. 2002). The central role of transcription factor Sox9 in the differentiation and maintenance of the chondrocyte phenotype is well established (de Crombrugghe et al. 2000). Through binding to tissue-specific enhancer elements, Sox9 is capable of activating cartilage collagen expression (Ng et al. 1997; de Crombrugghe et al. 2000). In the present study we show overlapping expression of Sox9 and type IIA collagen at sites of valvular and septal cardiogenesis, which suggests that Sox9 may function as transcriptional regulator of type II collagen also in the heart. However, the expression of Sox9 in the developing heart was more widespread than that of type IIA collagen. Temporally type IIA collagen was seen only during E9.5–E13.5 whereas Sox9 was also detected at later stages of heart development. The fact that nuclear Sox9 staining of the endocardial cushion disappeared faster than matrix staining for type IIA collagen can possibly be explained by the considerably shorter half-lives of transcription factors than collagens.
These data correlates well with previous data on the expression of Sox9 mRNA in the heart at E9.5–E16.5 (Ng et al. 1997). Interestingly, we localized Sox9 in the same areas where bone morphogenetic protein-2 (BMP-2) is expressed during embryonic heart development (Abdelwahid et al. 2001). BMP-2 has been shown to induce the expression of Sox9 in some prechondrogenic tissues as well as during skeletal repair (Zhu et al. 1999; Uusitalo et al. 2001). As type IIA collagen has previously been shown to bind TGF-β1 and BMP-2 and thereby regulate their activity (Zhu et al. 1999), a complex regulatory mechanism could be envisioned for the autoregulation of cartilage collagen production in the developing heart. These findings may also provide a novel way to interfere with the development of heart valves and septa as considerable experimental evidence has accumulated on the therapeutic modulation of chondrogenesis and type II collagen production by direct application of BMPs or through adenovirus-mediated delivery of BMP genes into target tissues. The present observations justify their experimental use also in the modulation of cardiac development.
References
Abdelwahid E, Rice D, Pelliniemi J, Jokinen E (2001) Overlapping and differential localization of Bmp-2, Bmp-4, Msx-2 and apoptosis in the endocardial cushion and adjacent tissues of the developing mouse heart. Cell Tissue Res 305:67–78
Bishop SE, Laurent GJ (1995) Collagen turnover and its regulation in the normal and hypertrophying heart. Eur Heart J 16(suppl C):38–44
Borg TK, Raso DS, Terracio L (1990) Potential role of the extracellular matrix in postseptation development of the heart. Ann N Y Acad Sci 588:87–92
Brewton RBG, Wright DW, Mayne R (1991) Structural and functional comparison of type IX collagen-proteoglycan from chicken cartilage and vitreous humor. J Biol Chem 266:4752–4757
Bridgewater LC, Lefebvre V, de Crombrugghe B (1998) Chondrocyte-specific enhancer elements in the Col11a2 gene resemble the Col2a1 tissue-specific enhancer. J Biol Chem 273:14998–15006
Burgeson RE, Nimni ME (1992) Collagen types. Molecular structure and tissue distribution. Clin Orthop 282:250–272
Carver W, Terracio L, Borg TK (1993) Expression and accumulation of interstitial collagen in the neonatal rat heart. Anat Rec 236:511–520
Cheah KSE, Lau ET, Au PKC, Tam PPL (1991) Expression of the mouse α1(II) gene is not restricted to cartilage during development. Development 111:945–953
Cheah KSE, Wong S, Ng L-J, Tam P (2002) An essential role for type IIA procollagen in heart development. In: XVIIIth Federation of European Connective Tissue Societies (FECTS) Meeting, Brighton, UK, 27–31 July 2002
Chirgwin JM, Przybyla AE, MacDonald RJ, Rutter WJ (1979) Isolation of biologically active ribonucleic acid from sources enriched in ribonuclease. Biochemistry 1:5294–5299
de Crombrugghe B, Lefebvre V, Behringer RR, Bi W, Murakami S, Huang W (2000) Transcriptional mechanisms of chondrocyte differentiation. Matrix Biol 19:389–394
Elima K, Metsäranta M, Kallio J, Perälä M, Eerola I, Garofalo S, De Grombrugghe, Vuorio E (1992) Specific hybridization probes for mouse type α2(IX) and α1(X) collagen mRNAs. Biochim Biophys Acta 1130:78–80
Joronen K, Salminen H, Glumoff V, Savontaus M, Vuorio E (2000) Temporospatial expression of tissue inhibitors of matrix metalloproteinases-1, -2 and -3 during development, growth and aging of the mouse skeleton. Histochem Cell Biol 114:157–165
Kosher RA, Solursh M (1989) Widespread distribution of type II collagen during embryonic chick development. Dev Biol 131:558–566
Lamers WH, Moorman AF (2002) Cardiac septation: a late contribution of the embryonic primary myocardium to heart morphogenesis. Circ Res 26;91:93–103
Li SW, Prockop DJ, Helminen H, Fässler R, Lapveteläinen T, Kiraly K, Peltarri A, Arokoski J, Lui H, Arita M, Khillan JS (1995) Transgenic mice with targeted inactivation of the Col2α1 gene for collagen II develop a skeleton with membranous and periosteal bone but no endochondral bone. Genes Dev 9:2821–2830
Linsenmayer TF, Hendrix MJ (1980) Monoclonal antibodies to connective tissue macromolecules: type II collagen. Biochem Biophys Res Commun 92:440–446
Little CD, Rongish BJ (1995) The extracellular matrix during heart development. Experientia 51:873–82
Liu CY, Olsen BR, Kao WW (1993) Developmental patterns of two alpha 1(IX) collagen mRNA isoforms in mouse. Dev Dyn 198:150–157
Lui VC, Ng LJ, Nicholls J, Tam PP, Cheah KS (1995) Tissue-specific and differential expression of alternative spliced α1(II) collagen mRNAs in early human embryos. Dev Dyn 203:198–211
Markwald R, Eisenberg C, Eisenberg L, Trusk T, Sugi Y (1996) Epithelial–mesenchymal transformations in early avian heart development. Acta Anat (Basel) 156:173–186
Mendler M, Eich-Bender SG, Vaughan L, Winterhalter KH, Brucner P (1989) Cartilage contains mixed fibrils of collagen types II, IX, and XI. J Cell Biol 108:191–197
Mertin S, McDowall SG, Harley VR (1999) The DNA-binding specificity of SOX9 and other SOX proteins. Nucleic Acids Res 27:1359–1364
Metsäranta M, Toman D, De Crombrugghe B, Vuorio E (1991) Specific hybridization probes for mouse type I, II, III and IX collagen mRNAs. Biochim Biophys Acta 1089:241–243
Nah HD, Upholt WB (1991) Type II collagen mRNA containing an alternative spliced exon predominates in the chick limb prior to chondrogenesis. J Biol Chem 266:23446–23452
Nakagawa M, Terracio L, Carver W, Birkedal-Hansen H, Borg TK (1992) Expression of collagenase and IL-12 in developing rat hearts. Dev Dyn 195:87–99
Ng Lj, Tam PP, Cheah KS (1993) Preferential expression of alternative spliced mRNAs encoding type II procollagen with cysteine-rich aminopropeptide in differentiating cartilage and nonchondrogenic tissues during early mouse development. Dev Biol 159:403–417
Ng LJ, Wheatley S, Muscat GE, Conway-Campbell J, Bowles J, Wright E, Bell DM, Tam PP, Cheah KS, Koopman P (1997) SOX9 binds DNA, activates transcription, and coexpresses with type II collagen during chondrogenesis in the mouse. Dev Biol 183:108–121
Oxford JT, Doege KJ, Morris NP (1995) Alternative exon splicing within the amino-terminal nontriple-helical domain of the rat proα1(XI) collagen gene generates multiple forms of the mRNA transcript which exhibit tissue dependent variations. J Biol Chem 270:9478–9485
Perälä M, Savontaus M, Metsaranta M, Vuorio E (1997) Developmental regulation of mRNA species for types II, IX and XI collagens during mouse embryogenesis. Biochem J 324:209–216
Pihlajamaa T, Perala M, Vuoristo MM, Nokelainen M, Bodo M, Schulthess T, Vuorio E, Timpl R, Engel J, Ala-Kokko L (1999) Characterization of recombinant human type IX collagen. Association of alpha chains into homotrimeric and heterotrimeric molecules. J Biol Chem 274:22464–22468
Potocki L, Abuelo D, Oyer C (1995) Cardiac malformation with two infants with hypochondrogenesis. Am J Med Genet 59:295–299
Salminen H, Vuorio E, Saamanen AM (2001) Expression of Sox9 and type IIA procollagen during attempted repair of articular cartilage damage in a transgenic mouse model of osteoarthritis. Arthritis Rheum 44:947–955
Sandberg M, Vuorio E (1987) Localization of types I, II, and III collagen mRNAs in developing human skeletal tissues by in situ hybridization. J Cell Biol 104:1077–1088
Sandberg MM, Hirvonen HE, Elima KJM, Vuorio EI (1993) Co-expression of collagens type II and XI and alternative splicing of exon 2 of collagen II in several developing human tissues. Biochem J 294:595–602
Savontaus M, Ihanamäki T, Metsäranta M, Sandberg-Lall M, Vuorio E (1997) Localization of type II collagen mRNAs isoforms in the developing eyes of normal and transgenic mice with a mutation in type II collagen gene. Invest Ophthalmol Vis Sci 38:930–942
Savontaus M, Ihanamäki T, Perälä M, Metsäranta M, Sandberg-Lall M, Vuorio E (1998) Expression of type II and IX collagen isoforms during normal and pathological cartilage and eye development. Histochem Cell Biol 110:149–159
Smith G Jr, Brandt KD (1992) Hypothesis: can type IX collagen "glue" together intersecting type II fibers in articular cartilage matrix? A proposed mechanism. J Rheumatol 19:14–17
Swiderski R, Daniels K, Jensen K, Solursh M (1994) Type II collagen is transiently expressed during avian cardiac valve morphogenesis. Dev Dyn 200:294–304
Thorogood P, Bee J, von der Mark K (1986) Transient expression of collagen type II at epitheliomesenchymal interfaces during morphogenesis of the cartilaginous neurocranium. Dev Biol 116:497–509
Uusitalo H, Hiltunen A, Ahonen M, Gao TJ, Lefebvre V, Harley V, Kahari VM, Vuorio E (2001) Accelerated up-regulation of L-Sox5, Sox6, and Sox9 by BMP-2 gene transfer during murine fracture healing. J Bone Miner Res 16:1837–1845
Webb S, Brown NA, Anderson RH (1998) Formation of the atrioventricular septal structures in the normal mouse. Circ Res 82:645–656
Wood A, Ashhurst DE, Corbett A, Thorogood P (1991) The transient expression of type II collagen at tissue interfaces during mammalian craniofacial development. Development 111:955–968
Ylä-Herttuala S, Rosenfeld ME, Parthasarathy S, Glass CK, Sigal E, Witztum JL, Steinberg D (1990) Colocalization of 15-lipoxygenase mRNA and protein with epitopes of oxidized low density lipoprotein in macrophage-rich areas of atherosclerotic lesions. Proc Natl Acad Sci U S A 87:6959–6963
Zhu Y, Oganesian A, Keene DR, Sandell LJ (1999) Type IIA procollagen containing the cysteine-rich amino propeptide is deposited in the extracellular matrix of prechondrogenic tissue and binds to TGF-beta1 and BMP-2. J Cell Biol 144:1069–1080
Acknowledgements
The authors are grateful to M. Lakkisto and T. Oivanen for expert technical assistance. This study was financially supported by the Academy of Finland (project number 52940) and the Finnish Heart Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rahkonen, O., Savontaus, M., Abdelwahid, E. et al. Expression patterns of cartilage collagens and Sox9 during mouse heart development. Histochem Cell Biol 120, 103–110 (2003). https://doi.org/10.1007/s00418-003-0549-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00418-003-0549-9