Abstract
Purpose
Resting energy expenditure (REE) determination is of high relevance to avoid both overfeeding and underfeeding. We conducted an observational study to determine the impact of early exercise on energy requirements to adjust caloric intake accordingly in critically ill patients.
Methods
This was a prospective observational study conducted in an intensive care unit in 49 hemodynamically stable critically ill patients and 15 healthy volunteers. Indirect calorimetry (IC) was performed for 15 min at baseline during resting conditions, and then continuously recorded during 30 min of cycling at 0, 3, or 6 watts (W), followed by a 15-min resting period. REE determined by IC was compared with predictive formulas and correlated with several biomarkers. The energy cost of early exercise was compared between critically ill patients and healthy volunteers.
Results
In patients, REE determined by IC was higher than predicted by Harris–Benedict (29 ± 31 %, p < 0.001) and Fleisch equations (23 ± 31 %, p < 0.001) but lower than predicted by the Faisy–Fagon equation for ventilated patients (16 ± 19 %, p < 0.05). Differences between Harris–Benedict predictions and IC determination were positively correlated with C-reactive protein (CRP) in patients with sepsis (r = 0.51, p = 0.003). During a similar exercise, VO2 increase in patients was higher when compared with healthy volunteers at 3 W, close to significant at 6 W, and not present in the passive group.
Conclusions
The critically ill have increased REE according to inflammation defined by CRP. Increased energy requirement for physical activity was only present for active exercise and seems to differ from that in the healthy population. For the exercise duration and intensity tested, nutritional adjustment is not indicated.
Similar content being viewed by others
Introduction
Nutrition of critically ill patients remains a matter of controversy. Indeed, the amount of energy to provide and the optimal timing of nutrition are not definitively established [1]. However, overfeeding and underfeeding generate deleterious consequences [2–6]. One of the goals of nutrition in this population is to preserve muscular mass during the hypercatabolic phase of critical illness [7], which otherwise induces functional impairment and the need for prolonged rehabilitation [8]. In this context, early exercise [9–11] could constitute an additional intervention to limit muscle wasting if combined with adequate feeding. Despite an expected increase in energy expenditure (EE) during exercise there is currently no recommendation for adjusting caloric intake in critically ill patients undergoing early physical therapy. In the healthy population energy cost induced by exercise can be accurately measured by means of a steady state effort potency. VO2 measurement during exercise is more valid at lower exercise intensity and higher duration for an accurate assessment of the aerobic component during the increase of metabolism. Indeed, the assessment of EE during exercise is valid only when anaerobic energy involved in the exercise is negligible [12, 13]. In healthy subjects, exercise-induced EE can be easily predicted on the basis of intensity [14]. Since the literature support early mobilization as an efficient intervention having an impact on functional outcome [15], our main objective was to determine the impact of exercise on energy requirements by measuring EE by indirect calorimetry (IC) at different intensities [16].
Methods
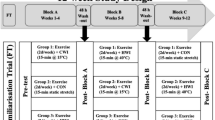
Study design
A prospective observational study was conducted in the intensive care unit at Saint Luc University Hospital for two periods. Adult patients were eligible 24 h after ICU admission if hemodynamically stable with or without vasopressor requirement. Non-inclusion criteria were limitation for cycling movement (orthopedic surgery, morbid obesity), agitation, and technical limitation for IC [17] such as inspired oxygen fraction more than 50 % in ventilated patients, oxygen administration in non-ventilated patients, and bronchopleural leaks. Additionally healthy volunteers served as controls.
Informed consent was signed by the subjects or next to kin for unconscious patients. The protocol was approved by the local biomedical ethics committee agreeing with the principles laid down in the Declaration of Helsinki.
Protocol development
Patients were consecutively included during two study periods. On the basis of preliminary observations, the 6-W target for active exercise had been initially selected. However, after initiating the study, it was realized that several patients were unable either to reach or maintain such a potency. For this reason, it was decided to test an intermediary potency in an additional arm at 3 W. Patients were evaluated by the same physiotherapist for their ability to perform exercise without any change in sedation. For awake patients, leg muscular strength was tested. Patients were considered appropriate for the active physical exercise arm when each leg strength was sufficient to resist gravity and oppose some resistance (more than 3 on the Medical Research Council scale) [18]. Non-awake patients or those unable to perform active exercise were enrolled in the passive arm.
Because ideal conditions for IC have to be strictly controlled to ensure reliable measurement [19, 20], patients and healthy volunteers had to satisfy the following criteria: (1) recording after a period of 4–5 h after meals or bolus of enteral feeding; (2) a comfortable positioning and environment with room temperature close to 25 °C; (3) a respiratory quotient (RQ) between 0.67 and 1.3, because outside these ranges IC measurement is not guaranteed [21]; (4) a minimal 30-min rest period; (5) abstention from moderate physical activity before; (6) a minimum of a 12-h period without smoking and coffee consumption. IC was performed with a validated device for this clinical setting (Deltatrac II Metabolic Monitor, Datex-Ohmeda, Helsinki, Finland) [22].
IC was conducted continuously during one complete hour divided into three periods. For the first period IC determination was recorded at rest during 15 min. During the second period lasting 30 min, the patient was asked to perform active or passive exercise with a motorized therapeutic trainer device for cycling movement. For the third period, determinations were collected during recovery from exercise.
During the active exercise, the patient was in a sitting position on a comfortable chair. The cycling exercise device was a Thera-Vital (Medica Medizintechnik GmbH, 88454 Hochdorf, Germany). Patients were asked to maintain a continuous stable exercise at a fixed potency of 6 W (Pat-6W) or 3 W (Pat-3W). For the passive arm (Pat-0W) patients were in a supine position with 30° of head inclination. The cycling exercise device (MOTOmed Letto2, RECK-Technik GmbH & Co. KG, 88422 Betzenweiler, Germany) was programmed at a fixed velocity of 20 rpm. To prevent adverse events during exercise, all hemodynamic parameters and clinical signs were monitored. Stop criteria were used as previously reported [10, 23]. Healthy volunteers were randomly allocated to three different arms.
Data collection
Oxygen consumption (VO2), carbon dioxide production (VCO2), RQ, and measured resting energy expenditure (REE) were collected every minute. To ensure steady-state conditions, the first 5 min of IC recordings was discarded for each protocol period. Values were only considered if the coefficient of variation was less than 10 % for VO2, VCO2, and REE. Predictive equations were used to calculate theoretical estimations of EE. Anamnestic body weight was used for subjects with a BMI less than 25. Ideal body weight was determined for all subjects with a BMI of at least 25 [24]. Stress factor was calculated from the ratio between measured to predicted EE by the Harris–Benedict (HB) equation. In patients, hemodynamic and respiratory parameters were recorded before, during exercise, and during the recovery period. Blood analyses were extracted from routine monitoring on the day of study. Arterial blood lactate was collected before and after exercise.
Statistical analysis
For continuous variables, means ± SD or medians are reported. Normality was checked using the Kolmogorov–Smirnov test. Differences between groups were compared using a two-sided independent Student t test when appropriate; otherwise the Mann–Whitney–Wilcoxon test was performed. The relationship between variables was assessed using the Pearson correlation coefficient. The limits of agreement between various methods for comparing REE were analyzed using a Bland–Altman plot. Analyses were performed using SPSS software, version 20 (IBM, Chicago, IL) and Graphpad Prism 5.0 (GraphPad Software, La Jolla, CA). A p value of less than 0.05 was considered significant.
Results
Patients
Sixty patients were included. Eleven patients’ data were discarded because of unstable IC recording during the resting period. Ten additional patients were excluded from the final analysis because they were unable to perform their exercise. Physical exhaustion occurred in 3 patients before the requested time of 30 min which led to cessation of physical activity. Seven patients maintained exercise during all 30 min but were unable to reach the required potency. Furthermore, no adverse event was recorded among all patients.
Patients characteristics are presented in Table 1. Pressure support was the only ventilation mode. Sedation, when indicated, was achieved by propofol at median doses of 77.06 mg/h (17.2–201.7 mg/h). All patients had a normal body temperature at inclusion. Five untrained healthy volunteers were included in each of the three arms: median age was 38 (24–56) in Ctrl-0W, 29 (20–44) in Ctrl-3W, and 25 (22–28) in Ctrl-6W. The sex ratio (male/female) was 5:5 in Ctrl-6W, 4:5 in Ctrl-3W, and 3:5 in Ctrl-0W.
Baseline measurements
Measured baseline REE was compared to values obtained from two predictive equations (electronic supplementary material). REE determined by IC was higher than predicted by HB (29 ± 31 %, p < 0.001) and Fleisch equations (23 ± 31 %, p < 0.001). Bland–Altman analysis showed differences between measured and predicted REE values by HB equation in all patients and in healthy volunteers (Fig. 1). For all patients the stress factor was 1.29 ± 0.31 (above 1.15 for 61 %, between 0.90 and 1.15 for 35 %, and less than 0.90 for only 4 %). In healthy volunteers the stress factor was 1.02 ± 0.19 (more than 1.15 in 20 %, between 0.90 and 1.15 in 53 %, and less than 0.90 in 27 %). The stress factor among patients with sepsis was 1.31 ± 0.32 and 1.27 ± 0.32 for the remaining critically ill. No patient was ventilated with a controlled mode, and the stress factor from mechanically ventilated patients was very similar to that in spontaneously breathing patients (1.27 ± 0.22 and 1.32 ± 0.38, respectively, p = 0.59). In mechanically ventilated patients, REE calculated by the Faisy–Fagon equation [25] was 16 ± 19 % above the value obtained by IC determination (p < 0.001) with a mean difference of 214 kcal/24 h (range −589 to 757 kcal/24 h).
Inflammation and EE
A correlation was found between measured REE for all 39 patients and CRP (r = 0.41, p = 0.004). In 31 patients with sepsis, this correlation was more pronounced (r = 0.47, p = 0.008). The difference between HB prediction and IC determination, standardized for body weight, was also positively correlated with CRP for the entire population (r = 0.42, p = 0.003) and in patients with sepsis (r = 0.51, p = 0.003) (Fig. 2). This correlation was even more pronounced for the first 3 days of sepsis (r = 0.72, p = 0.004, mean CRP = 18.8 ± 11.5 mg/dL) than after day 3 (r = 0.49, p = 0.04, mean CRP = 8.0 ± 7.8 mg/dL). In 18 patients without sepsis, the mean CRP was 8.9 ± 11.9 mg/dL without correlation (r = 0.28, p = 0.25). Others markers such as arterial lactate, APACHE II, and SOFA score were not correlated with REE measured by IC.
Effect of exercise
Exercise-induced changes in VO2 and EE differed significantly between patients and healthy volunteers at 3 W and were close to significance at 6 W (Fig. 3): increment in VO2 (ml/min) in Pat-3W vs Ctrl-3W was from 297 ± 117 to 400 ± 129 (38.5 ± 15.2 %) vs 268 ± 50 to 343 ± 48 (28.6 ± 6.9 %) (p = 0.04). Expressed in EE (kcal/24 h), this increment was from 2,006 ± 799 to 2,710 ± 877 (39.3 ± 16.3 %) vs 1,817 ± 346 to 2,308 ± 338 (28.0 ± 6.7 %) (p = 0.04) for the same population. In Pat-6W vs Ctrl-6W, VO2 increment was from 281 ± 85 to 425 ± 112 (53.3 ± 16.4 %) vs 243 ± 25 to 360 ± 43 (47.9 ± 7.0 %) (p = 0.20) and 1,900 ± 573 to 2,891 ± 755 (54.1 ± 16.7 %) vs 1,651 ± 182 to 2,465 ± 301 (49.3 ± 7.2 %) (p = 0.23) when expressed in EE (kcal/24 h). These observations remained present when VO2 and EE were standardized for body weight (Fig. 3b) or when expressed by metabolic equivalent (MET = 3.5 × VO2 (ml/min)/body weight). After active exercise, the time to return to VO2 and the EE resting condition was 3 ± 2 vs 2 ± 1 min for Pat-3W vs Ctrl-3W (p = 0.39), and 5 ± 3 vs 4 ± 1 min for Pat-6W vs Ctrl-6W (p = 0.89).
Exercise variation assessed by indirect calorimetry. a Evolution of VO2 assessed by indirect calorimetry. Ex exercise, R-5 5 min after exercise, R-10 10 min after exercise. Data are means ± mean error standard. b Rise of energy expenditure from rest time (T1) to exercise time (T2) (ΔEET2−T1) standardized by body weight. Pat-0W patients in passive group, Pat-3W patients performing 3-W exercise, Pat-6W patients performing 6-W exercise, Ctrl-0W healthy volunteers in passive group, Ctrl-3W healthy volunteers performing 3-W exercise, Ctrl-6W healthy volunteers performing 6-W exercise. Data are means ± mean error standard
In patients and volunteers undergoing passive exercise, no significant change in VO2 and EE from resting condition was observed during the 30 min of study period (Fig. 3a). Rise in VO2 (ml/min) observed in Pat-0W vs Ctrl-0W was from 244 ± 55 to 252 ± 57 (3.9 ± 9.1 %) vs from 225 ± 57 to 231 ± 66 (2.2 ± 5.2 %) (p = 0.60). The rise in EE (kcal/24 h) was from 1,672 ± 377 to 1,756 ± 356 (5.1 ± 6.9 %) vs 1,524 ± 399 to 1,565 ± 447 (2.0 ± 4.9 %) (p = 0.41), respectively. The results were not different between sedated or awake patients (data not shown).
Heart rate was increased with exercise by 12.8 ± 8.2 % (p < 0.001), 9.9 ± 4.7 % (p = 0.02), and 1.6 ± 4.7 % (p = 0.28) in Pat-6W, Pat-3W, and Pat-0W groups, respectively. Respiratory rate variations were 30.3 ± 27.2 % (p < 0.001) in Pat-6W, 16.8 ± 14.9 % (p = 0.03) in Pat-3W, and 1.4 ± 9.8 % (p = 0.59) in Pat-0W groups. Mean arterial pressure (mmHg) before and during exercise was 86 ± 15 vs 93 ± 18 (p = 0.36) in Pat-6W, 81 ± 11 vs 87 ± 11 (p = 0.23) in Pat-3W, and 77 ± 13 vs 78 ± 11 (p = 0.79) in Pat-0W groups. To investigate the impact upon myocardial work, rate–pressure product (RPP) was calculated as the product of peak systolic blood pressure and heart rate at rest vs exercise [26]. RPP was at 11,715.4 ± 4,511.6 vs 14,583.6 ± 5,251.4 (p < 0.001) for Pat-6W, 9,641.4 ± 2,336.8 vs 11,769.0 ± 3,230.4 (p = 0.02) for Pat-3W, and 10,362.4 ± 2,049.6 vs 10,808.1 ± 1,696.7 (p = 0.14) in Pat-0W.
In all patients VO2 changes induced by exercise were positively correlated with values from RPP (r = 0.70, p = 0.0001), heart rate (r = 0.50, p = 0.001), and respiratory rate (r = 0.76, p < 0.0001). In both active and passive groups, blood lactate was not modified.
Discussion
This study demonstrated that EE predicted by two common accepted equations is underestimated when compared with IC in the critically ill. We observed a significant correlation between a common biomarker of inflammation, CRP, and REE. Finally the energy cost induced by exercise was surprisingly more elevated in critically ill patients when compared with healthy volunteers and far above predictions.
REE determined by IC has been regularly demonstrated to be superior when compared with predicted values in critically ill patients [27]. This is not surprising because predictive equations were derived from a healthy population. Stress factors were very similar to the ones described by other authors in septic patients [28]. In mechanically ventilated patients, a stress factor of 1.34 or 1.32 has been described by others authors [28, 29], but ventilator mode and sedation were not specified. In another study showing a predominance of normal to reduced metabolism in critically ill patients, all patients with spontaneous mechanical ventilation and consequently all awake patients were excluded [30]. Sedation and mechanical ventilation have been identified as factors decreasing REE [28, 31]. In our study, we only used pressure support with low sedation levels and the calculated stress factor was similar to the observed stress factor in a spontaneously breathing population. The absence of difference between mechanically ventilated and spontaneous breathing patients has already been described [32]. The higher REE in our study when using the Faisy–Fagon equation compared with IC could be explained by a difference in minute ventilation. Indeed this equation takes into account minute ventilation generally being lower with a controlled mode of mechanical ventilation than a spontaneous mode.
Increase in serum CRP is positively correlated with elevated REE. This relation was already observed in cancer patients losing weight [33], and an association between serum CRP and elevated REE was found in another trial including a similar population [34]. This strongly suggests that the inflammatory response contributes to metabolism alterations in resting conditions. This observation is not surprising, but this correlation has never been described in the critically ill. This simple inflammation marker could be used to adapt the stress factor and help clinicians to adjust caloric intake when IC is not accessible or cannot be performed. Indeed, any serum CRP increase of 1 mg/dL was associated with 0.32 kcal/kg body weight (CI 95% 0.12–0.52) above values predicted by the HB equation.
Physical mobilization is now recommended during critical illness [15], but data regarding the energy cost are scarce. Our study shows that negligible energy cost is detected in patients undergoing passive exercise. Patients in the passive group were older, more critically ill, and more frequently mechanically ventilated. In this fragile population our goal is to prevent additional adverse events induced by exercise. Our results showed that 30 min of continuous passive exercise with a motorized device did not induce an additional stress because it was not associated with alteration in VO2, hemodynamics, or hyperlactatemia. This is in accordance with a recent case series showing that passive exercise in sedated and mechanically ventilated patients did not modify hemodynamic or metabolic parameters [35]. The main difference with our study is that we found similar observations without sedation, too. Indeed, it can be argued that sedative agents attenuate metabolic or hemodynamic response during exercise, but our results do not support this concept.
The absolute energy cost associated with active exercise was higher in critically ill patients than in volunteers for the same effort. This has never been shown previously in critically ill patients and raises numerous questions.
In patients, VO2 increase secondary to exercise is expected to be positively correlated with an increase in breathing and cardiac workload. Even if energy cost associated with exercise was less than 2 METs, it is easy to consider that patients need to increase respiratory workload. They eventually use accessory respiratory muscles because they are potentially close to VO2 max during illness and display skeletal muscle atrophy very early [36, 37]. Hemodynamic stress is reflected at baseline using RPP as an index of relative cardiac work. RPP at baseline was already higher in our patients compared with the healthy population described to be around 6,000 at rest and with an expected increase to fivefold during exercise. In our study, this value rises significantly, but less than values described in subjects with obstructive coronary artery disease [38]. We observed that 29 % of patients were unable to complete or maintain the exercise despite it being very light. It is likely that placing patients in a sitting position followed by a cycling exercise for 30 min could be a tremendous effort for the weakest patients. In this way, patients performing the 6-W exercise displayed a higher variability probably related to exercise intensity. Indeed, reaching and maintaining the requested 6-W target was more difficult to achieve, leading to an important variability and the loss of statistical significance. However, the trend and difference between critically ill patients and controls were maintained. Furthermore, it is important to consider that the anaerobic threshold was not reached because lactate at the end of exercise remained unchanged in all groups.
Finally the total amount of calories consumed by one session of cycling movement is limited and does not justify an increment of nutrition intake. However for prolonged exercise or greater efforts, this increment could reach significant values and augment the negative balance already present in critically ill patients [39]. This can not be answered by our study. Furthermore, our data confirm that static equations are not appropriate tools to adjust energy delivery.
Some limitations should be recognized. First, age was different between patients and controls. Despite this difference, exercise intensity was identical in both groups. Second, each individual patient was not investigated at the different intensity levels because both arms were performed during distinct periods. Moreover, performing both intensity levels would have been an exhausting exercise for some patients and therefore difficult to achieve on the same day. Also, the metabolic conditions could change daily and our goal was to assess the EE induced by exercise at the early stage of critical illness. Lastly, the magnitude of exercise expressed in watts remains an estimation.
In conclusion this study confirms that REE in the critically ill determined by IC is higher compared with predictive equations. Moreover, the equation established for mechanically ventilated patients overestimates REE in our patients. REE seems to be, at least partially, well correlated with the degree of inflammation evaluated by CRP. In this way, moderate active physical exercise in critically ill patients is associated with an increased EE compared with healthy volunteers. Finally passive physiotherapy and short-duration active mobilization do not require nutritional adjustment, but the impact of prolonged active mobilization should be further investigated.
References
Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, Vlasselaers D, Debaveye Y, Desmet L, Dubois J, Van Assche A, Vanderheyden S, Wilmer A, Van den Berghe G (2011) Early versus late parenteral nutrition in critically ill adults. N Engl J Med 365:506–517
Klein CJ, Stanek GS, Wiles CE III (1998) Overfeeding macronutrients to critically ill adults: metabolic complications. J Am Diet Assoc 98:795–806
Villet S, Chiolero RL, Bollmann MD, Revelly JP, Cayeux MC, Delarue J, Berger MM (2005) Negative impact of hypocaloric feeding and energy balance on clinical outcome in ICU patients. Clin Nutr 24:502–509
Rubinson L, Diette GB, Song X, Brower RG, Krishnan JA (2004) Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit Care Med 32:350–357
Singer P, Anbar R, Cohen J, Shapiro H, Shalita-Chesner M, Shaul L, Grozovski E, Theilla M, Frishman S, Madar Z (2011) The tight calorie control study (TICACOS): a prospective, randomized, controlled pilot study of nutritional support in critically ill patients. Intensive Care Med 37:601–609
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK (2009) The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 35:1728–1737
Biolo G (2013) Protein metabolism and requirements. World Rev Nutr Diet 105:12–20
Fletcher SN, Kennedy DD, Ghosh IR, Misra VP, Kiff K, Coakley JH, Hinds CJ (2003) Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med 31:1010–1012
Burtin C, Clerckx B, Robbeets C, Ferdinande P, Langer D, Troosters T, Hermans G, Decramer M, Gosselink R (2009) Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med 37:2499–2505
Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, Schmidt GA, Bowman A, Barr R, McCallister KE, Hall JB, Kress JP (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882
Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, Ross A, Anderson L, Baker S, Sanchez M, Penley L, Howard A, Dixon L, Leach S, Small R, Hite RD, Haponik E (2008) Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med 36:2238–2243
Scott CB, Fountaine C (2013) Estimating the energy costs of intermittent exercise. J Hum Kinet 38:107–113
Reis VM, Junior RS, Zajac A, Oliveira DR (2011) Energy cost of resistance exercises: an update. J Human Kinet 29A:33–39
McArdles WD (2007) Exercise physiology: energy, nutrition, and human performance. Lippincott Williams & Wilkins, London
Gosselink R, Bott J, Johnson M, Dean E, Nava S, Norrenberg M, Schönhofer B, Stiller K, van de Leurr H, Vincent JL (2008) Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med 34:1188–1199
Hickmann C, Roeseler J, Castanares-Zapatero D, Wittebole X, Mongodin A, Bialais E, Laterre PF (2011) Energy cost of early physical therapy in critically ill patients: a pilot study. Réanimation 21:86–89 (abstract)
Vohra SB, Keegan MA, Campbell IT, McGuinness S (1995) Practical limitations of the Deltatrac indirect calorimeter. Clin Nutr 14:155–161
Bittner EA, Martyn JA, George E, Frontera WR, Eikermann M (2009) Measurement of muscle strength in the intensive care unit. Crit Care Med 37:S321–S330
Haugen HA, Chan LN, Li F (2007) Indirect calorimetry: a practical guide for clinicians. Nutr Clin Pract 22:377–388
Compher C, Frankenfield D, Keim N, Roth-Yousey L (2006) Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc 106:881–903
McClave SA, Lowen CC, Kleber MJ, McConnell JW, Jung LY, Goldsmith LJ (2003) Clinical use of the respiratory quotient obtained from indirect calorimetry. J Parenter Enteral Nutr 27:21–26
Tissot S, Delafosse B, Bertrand O, Bouffard Y, Viale JP, Annat G (1995) Clinical validation of the Deltatrac monitoring system in mechanically ventilated patients. Intensive Care Med 21:149–153
Bourdin G, Barbier J, Burle JF, Durante G, Passant S, Vincent B, Badet M, Bayle F, Richard JC, Guérin C (2010) The feasibility of early physical activity in intensive care unit patients: a prospective observational one-center study. Respir Care 55:400–407
Berger MM, Pichard C (2012) Best timing for energy provision during critical illness. Crit Care 16:215
Faisy C, Guerot E, Diehl JL, Labrousse J, Fagon JY (2003) Assessment of resting energy expenditure in mechanically ventilated patients. Am J Clin Nutr 78:241–249
Gobel FL, Norstrom LA, Nelson RR, Jorgensen CR, Wang Y (1978) The rate-pressure product as an index of myocardial oxygen consumption during exercise in patients with angina pectoris. Circulation 57:549–556
Weissman C, Kemper M, Askanazi J, Hyman AI, Kinney JM (1986) Resting metabolic rate of the critically ill patients: measured versus predicted. J Anesthesiol 64:673–679
Barak N, Wall-Alonso E, Sitrin MD (2002) Evaluation of stress factors and body weight adjustments currently used to estimate energy expenditure in hospitalized patients. J Parenter Enteral Nutr 26:231–238
Swinamer DL, Grace MG, Hamilton SM, Jones RL, Roberts P, King EG (1990) Predictive equation for assessing energy expenditure in mechanically ventilated critically ill patients. Crit Care Med 18:657–661
Japur CC, Penaforte FRO, Chiarello PG, Monteiro JP, Vieira MNCM, Basile-Filho A (2009) Harris-Benedict equation for critically ill patients: are there differences with indirect calorimetry? J Crit Care 24:628e1–628e5
Chiolero R, Revelly JP, Tappy L (1997) Energy metabolism in sepsis and injury. Nutrition 13:45–51
Kreymann G, Grosser S, Buggisch P, Gottschall C, Matthaei S, Greten H (1993) Oxygen consumption and resting metabolic rate in sepsis, sepsis syndrome, and septic shock. Crit Care Med 21:1012–1019
Johnson G, Sallé A, Lorimier G, Laccourreye L, Enon B, Blin V, Jousset Y, Arnaud JP, Malthièry Y, Simard G, Ritz P (2008) Cancer cachexia: measured and predicted resting energy expenditures for nutritional needs evaluation. Nutrition 24:443–450
Falconer JS, Fearon KC, Plester CE, Ross JA, Carter DC (1994) Cytokines, the acute-phase response, and resting energy expenditure in cachectic patients with pancreatic cancer. Ann Surg 219:325–331
Camargo Pires-Neto R, Fogaça Kawaguchi YM, Sayuri Hirota A, Fu C, Tanaka C, Caruso P, Park M, Ribeiro Carvalho CR (2013) Very early passive cycling exercise in mechanically ventilated critically ill patients: physiological and safety aspects—a case series. PLoS One 8:e74182
Gamrin L, Andersson K, Hultman E, Nilsson E, Essén P, Wernerman J (1997) Longitudinal changes of biochemical parameters in muscle during critical illness. Metabolism 47:756–762
Poulsen JB, Møller K, Jensen CV, Weisdorf S, Kehlet H, Perner A (2011) Effect of transcutaneous electrical muscle stimulation on muscle volume in patients with septic shock. Crit Care Med 39:456–461
Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, Froelicher VF, Leon AS, Piña IL, Rodney R, Simons-Morton DA, Williams MA, Bazzarre T (2001) Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 104:1694–1740
Weissman C, Kemper M, Damask MC, Askanazi J, Hyman AI, Kinney JM (1984) Effect of routine intensive care interactions on metabolic rate. Chest 86:815–818
Acknowledgments
We thank intensive care team members for their participation as healthy volunteers and nursing team for their substantial collaboration.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Energy expenditure in patients with sepsis is correlated with inflammation. Energy cost induced by early active exercise is higher in the critically ill compared with healthy volunteers.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hickmann, C.E., Roeseler, J., Castanares-Zapatero, D. et al. Energy expenditure in the critically ill performing early physical therapy. Intensive Care Med 40, 548–555 (2014). https://doi.org/10.1007/s00134-014-3218-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3218-7