Abstract
Rationale
Permissive hypercapnia is established in lung injury management. Therapeutic hypercapnia causes benefit or harm, depending on the context. Ventilator-associated lung injury has a wide spectrum of candidate mechanisms, affording multiple opportunities for intervention such as hypercapnia to exert benefit or harm.
Objectives
To confirm (1) that hypercapnia attenuates in vivo ventilator-induced lung injury (VILI); (2) biological plausibility of such protection (e.g., dose-response, time series, inflammatory profile); and (3) that the associated biochemical events are consistently beneficial.
Methods
A mouse model of VILI was established in vivo. Injurious ventilation was established, hypercapnia applied and markers of inflammation measured.
Measurements
Lung injury was quantified by gas exchange, elastance, microvascular leak, histology and levels of cytokines and eicosanoids, cyclooxygenase and tissue nitrotyrosine.
Main results
Injurious ventilation caused significant lung injury (mechanics, microvascular leak, histology) and release of inflammatory cytokines, chemokines and eicosanoids. Hypercapnia attenuated these responses, with dose-response and time-dependent effects. No adverse effects of hypercapnia were observed in controls. Hypercapnia suppressed the transcription (mRNA) and translation (protein) of the major inducible prostanoid-generating enzyme (COX-2), but the effects on the downstream eicosanoids were modest. However, hypercapnia significantly increased lung tissue nitrotyrosine—at PaCO2 levels that were protective.
Conclusions
Hypercapnia provided consistent and biologically plausible in vivo protection against VILI, but elevated lung tissue levels of nitro-tyrosine as previously described in sepsis. Clinicians and those designing clinical trials need to be aware of the potential for detrimental effects when using hypercapnia in order to balance benefits versus harm with this approach.
Similar content being viewed by others
Introduction
Permissive hypercapnia is the acceptance of elevated CO2 that results from the limitation of inspiratory tidal volume (or pressure) in patients receiving mechanical ventilation [1]. In this context, the most important principle of supportive therapy is to minimize lung injury induced by mechanical stretch, i.e., ventilator-associated lung injury. While lessening tidal volume (V T) is associated with improved patient survival [2], hypercapnia may have additional roles [3, 4]. First, the ‘permissive’ hypercapnia resulting from V T reduction may coincidentally improve survival, an effect that may be additive to the protective effects of reducing V T [5]. Second, the deliberate elevation of CO2, therapeutic hypercapnia [6], has been hypothesized to directly protect against organ injury, and this has been demonstrated experimentally [7–15]. However, while salutatory effects of CO2 have been identified, there are potentially serious adverse effects. These include pulmonary or intracranial hypertension [16, 17], as well as more recently described molecular and cellular alterations [18–24], such as injury from nitrogen-derived oxidants [22–24], and adverse protein modification of important enzyme systems (e.g., Na/K-ATPase) [25]. Such adverse events may explain recent reports of worsening progression of sepsis associated with hypercapnia [14, 20, 26].
Balancing adverse effects, a series of cellular and molecular processes that are considered beneficial in the context of injury have been observed with hypercapnia. Such processes include induction of Axl (an anti-apoptotic protein) in cultured umbilical vein endothelial cells [27], attenuation of NF-κB signaling in cultured pulmonary artery endothelial cells [28], inhibition of interleukin-8 release from isolated neutrophils [29], inhibition of xanthine oxidase ex vivo [7], activation of K-ATPase channels in vascular smooth muscle [30] and the in vivo inhibition of cytokine release [8, 12].
Whether any specific mechanism is pathogenic or protective may depend on the nature and timing of the injury and on the inflammatory milieu. For example, in experimental models of sepsis, hypercapnia can exert net harm [26]—or net benefit [14]—depending on trajectory of the infection. Indeed, in short-term sepsis models, nitrotyrosine formation (conventionally considered harmful) was increased with hypercapnia [19, 20, 31]. However, in ventilator-induced lung injury without sepsis, the reported effects of hypercapnia have so far been beneficial [8, 9, 11]—or neutral [32]—but not adverse.
In this study we sought: (1) to confirm that hypercapnic acidosis attenuates in vivo ventilator-induced lung injury, (2) to determine whether additional features of biological plausibility supported such protection (e.g., dose-response, time series, accompanying inflammatory profile) and (3) if hypercapnia would protect lung tissue biochemistry from changes associated with injurious ventilation.
Materials and methods
All experiments were performed according to the protocols approved by the Animal Care and Use Committee of the Research Institute at the Hospital for Sick Children, Toronto, Canada.
Animal experiments
C57BL/6 female mice (20–25 g, Charles River, St. Constant, Canada) were anesthetized (ketamine/xylazine 150/15 mg kg−1, IP), a tracheostomy was inserted, and they were ventilated using a computer-controlled small animal ventilator (SCIREQ, Flexivent, Montreal, Canada) [33] with the following settings, which do not cause vivo ventilator-induced lung injury (VILI) in the in vivo mouse lung over the time interval studied, in the absence of a pre-ventilation injury: V T 10 ml kg−1, PEEP 1.0 cmH2O, frequency 135 min−1, FiO2 0.75 and FiN2 0.25. Core temperature was maintained (36.5–38.0°C) and supplemental fluids and anesthesia administered as required throughout the experiment. Lung elastance was measured at baseline and hourly thereafter. Evans Blue (Sigma-Aldrich, Oakville, ON, Canada; 30 ml kg−1, IV) was given, and animals were randomized to receive injurious ventilation (V T 45 ml kg−1, PEEP 0 cmH2O, frequency 30–35 min−1) or control ventilation (V T 12 ml kg−1, PEEP 1 cmH2O, frequency 135 min−1), in the setting of either normocapnia (FiO2 0.75, FiCO2 0, balance N2) or hypercapnia (FiO2 0.75, FiCO2 0.12, balance N2). All of these ventilator settings are known, from pilot data, to result in normocapnia where FiCO2 is zero. Arterial blood gas measurements were performed at the end of each experiment and the animals killed by exsanguination. Bronchoalveolar lavage was followed by removal of the lungs en bloc, and the lung tissue retained (−80°C). Additional animals were studied to examine the effects of increasing concentrations of FiCO2 (0.05, 0.12, 0.25) with FiO2 0.75 and balance N2 in all cases. Pulmonary microvascular permeability was determined using a modification of the Evans’ Blue technique as previously described [34], where BAL concentration of Evans blue corrected for the presence of heme pigments [35].
Mediator assays
Bronchoalveolar lavage samples were analyzed for cytokines (interleukin-6, IL-6; keratinocyte chemoattractant factor, KC; macrophage chemoattractant protein-1, MCP-1), the soluble cell adhesion molecules (soluble vascular cell adhesion molecule, sV-CAM; soluble E-selectin) and matrix metallo-proteinase-9 (MMP-9), were measured with commercial ELISA kits (LINCOplex Kits, LINCO Research, St. Charles, MI), according to manufacturer’s instructions. In addition, TNFα bioactivity in BAL was measured with a murine fibroblast cytotoxicity assay [36], where cell death was assessed using the methylthiazoletetrazolium method [37]. Stable hydrolysis products of prostaglandins, leucotrienes and lipoxins were measured in total lung tissue by liquid chromatography–tandem mass spectrometry (LC–MS/MS) using an API4000 triple-quadruple mass spectrometer (MDS SCIEX, Concord, ON, Canada) [38].
Histopathology and immunohistochemistry
Right lungs were pressure fixed (10% buffered formalin, 20 cmH2O), serially sectioned from apex to base, randomly selected, stained with hematoxylin-eosin and examined by an observer blinded to experimental group. Paraffin tissue sections were deparaffinized, rehydrated, microwaved for antigen retrieval and incubated (3% H2O2) to quench endogenous peroxidase. Nonspecific adsorption was minimized (incubation with 10% goat serum) and the sections then incubated with primary anti-MPO polyclonal antibody, polyclonal anti-3-NT or with control solutions (buffer alone; non-specific purified rabbit IgG or blocking peptides). Specific labeling was detected with biotinylated goat anti-rabbit IgG, followed by incubation with avidin DH and biotinylated horseradish peroxidase and diaminobenzidine tetrahydrochloride as chromogen. Counterstaining was with hematoxylin.
Cyclooxygenase and nitrotyrosine protein
COX-2 and 3-nitrotyrosine (3-NT) protein expression was examined using Western blot analysis of lung tissue using polyclonal rabbit anti-mouse antibodies (Cayman Chemicals, Ann Arbor, MI), incubated with horseradish peroxidase-conjugated anti-rabbit IgG (BioRad, Mississauga, ON, Canada) and visualized by enhanced chemiluminescence (ECL, Amersham Biosciences, Piscataway, NJ); the data were normalized against the housekeeping protein GAPDH.
Cyclooxygenase mRNA
COX-2 mRNA expression was assessed on Northern blots of total mRNA isolated from lung tissue using TRIzol (Invitrogen, Burlington, ON, Canada), hybridized with a [32P]dCTP-labeled cDNA encoding mouse COX-2. Following stringent washing, COX-2 mRNA was visualized by autoradiography, and blots were stripped and reprobed with GAPDH for normalization.
Statistics
Data were analyzed using SigmaStat (version 2.0; Jandel Corporation, San Rafael, CA). Group comparisons were performed with ANOVA followed by Student-Newman-Keuls or t tests for parametric data, and with ANOVA on ranks followed by Dunn’s tests for non-parametric data. Significance was set at P < 0.05. Results are expressed as mean ± standard deviation (SD).
Results
Lung pathophysiology
Baseline animal weight and respiratory system compliance were comparable among the groups (Table 1). The blood gas and acid-base data at the end of the experiment confirmed hypercapnic acidosis in both hypercapnia groups, mild metabolic acidosis in the injurious ventilation/normocapnia group and close to normal acid-base status with protective ventilation/normocapnia (Table 1).
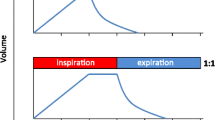
Elastance was similar among all groups at baseline and became significantly increased in the two injurious ventilation groups over time, but to a significantly lesser extent in the injurious ventilation/hypercapnia group (Fig. 1a). The order for final elevation in elastance was: injurious ventilation/normocapnia > injurious ventilation/hypercapnia > protective ventilation/normocapnia ≈ protective ventilation/hypercapnia. The same order of injury was reflected in lung microvascular leakage (BAL Evans’ Blue; Fig. 1b), as well as in the histologic appearance (Fig. 2a) and intensity of myeloperoxidase staining (Fig. 2b).
Serial elastance and microvascular leakage: injurious ventilation resulted in a progressive worsening in respiratory system elastance (vs. non-injurious ventilation; a). Addition of 12% CO2 to the inspired gas resulted in a smaller increase in elastance versus normocapnia. Injurious ventilation resulted in greater microvascular leak (BAL Evans’ Blue concentration; b), which was attenuated by hypercapnia. Data are means ± SD n = 13 injurious ventilation, n = 8 protective ventilation. *Injurious ventilation normocapnia versus all other groups (two-way repeated measures ANOVA on ranks, P < 0.001; Dunn’s test, P < 0.05)
Histology and myeloperoxidase: representative histologic sections (a hematoxylin and eosin (H&E) ×400; b myeloperoxidase immunoreactivity counterstained with H&E, ×400) indicates greatest injury in the injurious ventilation/normocapnia sections, less injury with injurious ventilation/hypercapnia and normal appearances with non-injurious ventilation (whether normocapnia or hypercapnia). (HM hyaline membrane, IC infiltrating cells, E edema.) MPO-immunoreactive (brown staining) cells include neutrophils and pulmonary alveolar macrophages (b)
In an additional group of experiments, a dose-response effect was also apparent wherein higher concentrations of added CO2 (0 vs. 5, 12 or 25% inspired CO2) were associated with incrementally better protection against injury in terms of elastance (Fig. 3a) and microvascular leakage (Fig. 3b).
Dose-response effects of CO2 on injury: injurious ventilation resulted in progressive worsening of respiratory system elastance during 3 h of ventilation (a). There was a dose-response effect whereby higher concentrations of inspired CO2 resulted in progressively more effective attenuation of injury over time (a). Similarly, higher doses of inspired CO2 resulted in less microvascular leakage at the end of 3 h of injurious ventilation (b). Data are means ± SD, 4–6 per group. *P < 0.05 (ANOVA on ranks)
Inflammatory mediators
The BAL fluid concentrations of several cytokines (interleukin-6, IL-6; keratinocyte chemoattractant factor, KC; macrophage chemoattractant protein-1, MCP-1) (Figure 1S), the soluble cell adhesion molecules (soluble vascular cell adhesion molecule, sV-CAM; soluble E-selectin) (Figure 2S) and matrix metallo-proteinase-9 (MMP-9) (Figure 2S) all mirrored the above patterns. Because TNFα is known to exhibit phasic responses to injurious ventilation [39], time-course experiments were performed to assess the activity over time, and hypercapnia attenuated both peaks (45 and 180 min) of TNFα activity (Figure 3S).
Cyclooxygenase and eicosanoids
The above cytokines mirrored the physiologic impact of injurious ventilation and the patterns of protection afforded by hypercapnic acidosis. A number of these mediators regulate the expression of cyclooxygenase (COX) enzymes, which are important proximal regulators of prostanoid synthesis. Prostanoids have been progressively implicated in the pathogenesis of acute lung injury [38], and because the acutely responsive (i.e., inducible) eicosanoid-producing enzyme in the lung is COX-2, the COX-2 enzyme protein level was measured. COX-2 protein was increased by injurious ventilation, and this increase was less in the presence of hypercapnia; as well, hypercapnia appeared to reduce the baseline COX-2 levels (Fig. 4a). Overall the order of lung tissue COX-2 protein levels was: injurious ventilation/normocapnia > injurious ventilation/hypercapnia > protective ventilation/normocapnia > protective ventilation/hypercapnia. In order to determine whether the increase in COX-2 protein represented new COX-2 synthesis, the expression of COX-2 mRNA was measured and found to be overwhelmingly induced by injurious ventilation; this effect was strongly attenuated by hypercapnia (Fig. 4b).
Tissue cyclooxygenase protein and mRNA: tissue COX-2 protein levels (Western blot) were increased by injurious ventilation, and the increase was attenuated by hypercapnia (a). A similar pattern was observed for tissue COX-2 mRNA levels (Northern blot, b). †Injurious ventilation normocapnia versus all other groups (ANOVA, P < 0.001; Student-Neuman-Keuls test P < 0.05); *hypercapnia versus all other groups (ANOVA, P < 0.001; Student-Neuman Keuls test P < 0.05)
However, despite the attenuation of COX-2 protein levels by hypercapnia, the levels of COX-2 products were only moderately suppressed. In addition, it was noted that arachidonic acid, the substrate for eicosanoid production, was also significantly lower in the presence of hypercapnia (Figure 4S).
Lung tissue nitrotyrosine
Sepsis models have frequently demonstrated increases in tissue nitrotyrosine levels. Injurious ventilation was associated with a modest increase in nitrotyrosine immunostaining (Fig. 5a) and increased detection of 3-nitrotyrosine on Western blot (Fig. 5b). However, despite otherwise overall protective effects, hypercapnia significantly increased the lung tissue nitrotyrosine load.
Lung tissue nitrotyrosine: injurious ventilation was associated with a modest increase in nitrotyrosine immunostaining (a) and increased detection of 3-nitrotyrosine on Western blot (b). However, despite otherwise overall protective effects, hypercapnia significantly increased the lung tissue nitrotyrosine load. *P < 0.05 hypercapnia versus normocapnia (unpaired t test)
Discussion
The current data confirm the protective effects of therapeutic hypercapnia initiated concurrently with injurious ventilation in an in vivo model of ventilator-induced lung injury, and characterize its effects on multiple mediators, including cytokines, eicosanoids and tissue nitration. The enhancing effect of hypercapnia on oxygenation may be due to amelioration of injury or to a direct enhancement of PaO2 (previously reviewed) [6].
Cytokine responses
The inflammatory cytokines assayed in the current study were chosen because of their strong association with ventilator-induced lung injury [40, 41] and the reliability of murine assays. The cytokine response mirrored the injury responses, and the TNFα responses were studied at several time points because of the known biphasic time course during high tidal volume ventilation [42]. In the current study, both the early and the late phases of TNFα elevation were inhibited by hypercapnia, such that the profile was similar to the control (un-injured) protocols in the current and previous [39] reports. The remaining cytokine responses were closely aligned with each other, and with the overall injury pattern, consistent with previous reports [40, 41]. The impact of hypercapnia was uniform among all assayed mediators.
Eicosanoids, injury and hypercapnia
Several of the cytokine mediators are important regulators of COX expression, which in turn regulates prostanoid synthesis. We measured tissue eicosanoid levels and found that hypercapnia attenuated the elevation of ‘core’ eicosanoid molecules (i.e., arachidonic acid, PGF2α, thromboxane B2). The BAL samples—assayed for a broader range of eicosanoids—revealed that although almost all classes were elevated by injurious ventilation (i.e., paralleled the degree of injury), the COX-2-dependent eicosanoids poorly paralleled the protection observed with hypercapnia.
In general, inflammatory prostanoids appear to be important in acute lung injury [43]. COX-2 is inducible and its expression increases following exposure to inflammatory mediators such as growth factors, cytokines and endotoxin [44], as well as stretch [38]. IL-1β, a proximal pro-inflammatory cytokine that is ubiquitously increased in ventilator-induced lung injury [40, 41], directly induces COX-2 via NF-κB [45]. Indeed, increased expression of COX-2 is mediated by several signaling pathways including cAMP, MAP-kinase and NF-κB [46], the latter being activated in ventilator-induced lung injury [47]. However, in the current study, despite hypercapnia-mediated suppression of COX-2 induction, substantial quantities of distal prostanoids were measured, indicating that the constitutive COX-1 may have a substitutive role in prostanoid generation in this model. Indeed, since the decreases in PGF2α and TXB2 are similar to the decrease in the COX substrate arachidonic acid, we cannot differentiate whether the decreases in prostanoid production under hypercapnia were due to the suppression of COX-2 or to suppression of arachidonic acid levels.
Mechanisms of hypercapnic protection
A small number of studies point to potential mechanisms of protection from injury associated with hypercapnic acidosis. The release of cytokines is an ubiquitous association of the development of almost all forms of acute lung injury [40, 41, 47]. In several studies demonstrating hypercapnic protection against lung injury, attenuation of cytokine release has been a consistent feature [8, 10, 12]. However, in such cases, it is not clear whether the inhibition of inflammatory mediators is a cause—or a consequence—of the lesser injury that occurred in the context of hypercapnia. One study has examined the release of pro-inflammatory cytokines in cultured leukocytes, in the absence of additional injury [29]. That study demonstrates that hypercapnia inhibits the release of interleukin-8 from stimulated leukocytes; such inhibition appears to be on the basis of increased intracellular H+, is dependent on intracellular carbonic anhydrase and is the converse of the effects observed with hypocapnic alkalosis [29]. Despite the consistency of the association between lung injury and elevated cytokines, there are significant doubts about the pathogenicity of cytokines in the development of ventilator-associated lung injury [48]. Thus, exploration of the effects of hypercapnia must extend beyond individual pro-inflammatory cytokines.
The IκB/NF-κB signaling pathway is a central pathway linking signal transduction with transcription regulation in sepsis [49] and mechanical stretch [47]. In the context of endotoxin-induced lung injury, hypercapnic acidosis has been shown to inhibit the translocation of NF-κB by stabilization of IκB [28]. Several additional pathways mediate ventilator-induced lung injury, including apoptosis and oxidant-induced injury; limited studies suggest hypercapnic acidosis may also affect such pathways [27].
Mechanisms of harm
In parallel with explorations of potential mechanisms of protection, several groups have reported on the molecular basis for how hypercapnia may cause harm. In the absence of sepsis—or any injury—increased levels of CO2 result in increased peroxynitration of surfactant protein-A, and the increased level of nitration is directly correlated with functional impairment (i.e. ability to aggregate lipids) [18]. Lange et al. [19] reported that increased CO2 resulted in higher levels of nitration of cultured epithelial cells—a phenomenon that was accentuated in the presence of pro-inflammatory cytokines—and suggested that the source of the increased nitration was linked to upregulation of nitric oxide synthase. In addition, CO2 promotes nitrotyrosine at the chemical level in that binding to peroxynitrite (ONOO) it forms an adduct (ONOOCO2 −), which promotes tyrosine nitration even more than peroxynitrite alone. Therefore, even if the levels of NOS, NO and superoxide are not elevated, the addition of CO2 will increase the propensity for nitrotyrosine formation. The same pattern of concern was reproduced in vivo in a follow-up study by Lange et al. [20], where hypoventilation resulted in worsening of LPS-induced lung injury, with an increased intensity of tissue nitration. Tissue nitration is usually an adverse development, as examples from the literature indicate that it is usually associated with a significant lack of protein function whether in the setting of hypercapnia [18] or otherwise. However, it is impossible to determine net benefit or harm from our overall measures of tissue nitration, since one could speculate that nitration and hence inhibition of pro-inflammatory or pro-apoptotic proteins might confer net benefit on the lung. In addition, peroxynitrate and nitrotyrosine have been reported to influence src family kinase activity, thus modifying intracellular signaling [50, 51], potentially influence lung injury. Finally, while tyrosine nitration is a marker of peroxynitrite formation, peroxynitrite itself has many effects beyond nitration of tyrosine. CO2 by forming the ONOOCO2 − adduct enhances nitration of tyrosine. While on balance nitrotyrosine would be expected to have negative effects on protein functions, elevated levels of peroxynitrite may be far more adverse in terms of, for example, lipid peroxidation, depletion of glutathione, inhibition of mitochondrial respiration and direct DNA damage in the absence of ONOOCO2 − formation [52].
Limitations and future studies
The in vivo mouse is naturally limited in terms of immediate applicability. Murine models, while invaluable for assay availability, knowledge of the genome and the ability to develop genetically modified models, possess fundamentally different physiological characteristics. In our mouse model, it should be noted that the PaO2 was higher than would be anticipated clinically; while it is not possible to rule out an additive or synergistic effect of hyperoxia with injurious ventilation, hyperoxia appears innocuous in the adult mouse (in contrast to neonatal rats). Nonetheless, they provide insights that are sometimes not otherwise possible. Subsequent investigation in this area could involve longer term survival or in vivo imaging [53] that could identify time course, trajectory and tissue-specificity of both inflammation and evolution of lung injury, as well as its inhibition by hypercapnia. For maximal relevance to clinical practice, application of hypercapnia after injury has become established will be important. The effects of peroxynitrate and tissue nitration are complex, and the net effect of increased nitrotyrosine formation in the hypercapnic setting is unknown. Considerable future work will be needed to determine the key target proteins, whether these proteins are activated or inhibited, and the net effect of these activity changes on lung injury.
Conclusion
The current report confirms that hypercapnia provides in vivo protection in a model of ventilator-induced lung injury, illustrates the pattern of responses of important regulatory mediators, identifies inconsistency regarding the eicosanoid profile and identifies the potentially harmful generation of nitrotyrosine formation. Thus, clinicians and those designing clinical trials need to be aware of the potential for detrimental effects when using hypercapnia, even in the absence of sepsis, in order to balance benefits versus harm with this approach.
References
Hickling KG, Walsh J, Henderson S, Jackson R (1994) Low mortality rate in adult respiratory distress syndrome using low-volume, pressure-limited ventilation with permissive hypercapnia: a prospective study. Crit Care Med 22:1568–1578
Hickling KG (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The acute respiratory distress syndrome network. N Engl J Med 342:1301–1308
Kregenow DA, Swenson ER (2002) The lung and carbon dioxide: implications for permissive and therapeutic hypercapnia. Eur Respir J 20:6–11
Laffey JG, Kavanagh BP (2000) Biological effects of hypercapnia (Review). Intens Care Med 26:133–138
Kregenow DA, Rubenfeld GD, Hudson LD, Swenson ER (2006) Hypercapnic acidosis and mortality in acute lung injury. Crit Care Med 34:1–7
Laffey JG, Kavanagh BP (1999) Carbon dioxide and the critically ill—too little of a good thing? (Hypothesis Paper). Lancet 354:1283–1286
Shibata K, Cregg N, Engelberts D, Takeuchi A, Fedorko L, Kavanagh BP (1998) Hypercapnic acidosis may attenuate acute lung injury by inhibition of endogenous xanthine oxidase. Am J Resp Crit Care Med 158:1578–1584
Halbertsma FJ, Vaneker M, Pickkers P, Snijdelaar DG, van Egmond J, Scheffer GJ, van der Hoeven HG (2008) Hypercapnic acidosis attenuates the pulmonary innate immune response in ventilated healthy mice. Crit Care Med 36:2403–2406
Sinclair SE, Kregenow DA, Lamm WJ, Starr IR, Chi EY, Hlastala MP (2002) Hypercapnic acidosis is protective in an in vivo model of ventilator-induced lung injury. Am J Respir Crit Care Med 166:403–408
Strand M, Ikegami M, Jobe AH (2003) Effects of high PCO2 on ventilated preterm lamb lungs. Pediatr Res 53:468–472
Broccard AF, Hotchkiss JR, Vannay C, Markert M, Sauty A, Feihl F, Schaller MD (2001) Protective effects of hypercapnic acidosis on ventilator-induced lung injury. Am J Respir Crit Care Med 164:802–806
Laffey JG, Jankov RP, Engelberts D, Tanswell AK, Post M, Lindsay T, Mullen JB, Romaschin A, Stephens D, McKerlie C, Kavanagh BP (2003) Effects of therapeutic hypercapnia on mesenteric ischemia-reperfusion injury. Am J Respir Crit Care Med 168:1383–1390
Laffey JG, Tanaka M, Engelberts D, Luo X, Yuan S, Keith Tanswell A, Post M, Lindsay T, Kavanagh BP (2000) Therapeutic hypercapnia reduces pulmonary and systemic injury following in vivo lung reperfusion. Am J Respir Crit Care Med 162:2287–2294
Chonghaile MN, Higgins BD, Costello J, Laffey JG (2008) Hypercapnic acidosis attenuates lung injury induced by established bacterial pneumonia. Anesthesiology 109:837–848
Ni Chonghaile M, Higgins BD, Costello JF, Laffey JG (2008) Hypercapnic acidosis attenuates severe acute bacterial pneumonia-induced lung injury by a neutrophil-independent mechanism. Crit Care Med 36:3135–3144
Feihl F, Perret C (1994) Permissive hypercapnia. How permissive should we be? Am J Resp Crit Care Med 150:1722–1737
Nunn JF (1987) Applied respiratory physiology. Butterworths, London, pp 235–283
Zhu S, Basiouny KF, Crow JP, Matalon S (2000) Carbon dioxide enhances nitration of surfactant protein A by activated alveolar macrophages. Am J Physiol Lung Cell Mol Physiol 278:L1025–L1031
Lang JD Jr, Chumley P, Eiserich JP, Estevez A, Bamberg T, Adhami A, Crow J, Freeman BA (2000) Hypercapnia induces injury to alveolar epithelial cells via a nitric oxide-dependent pathway. Am J Physiol Lung Cell Mol Physiol 279:L994–L1002
Lang JD, Figueroa M, Sanders KD, Aslan M, Liu Y, Chumley P, Freeman BA (2005) Hypercapnia via reduced rate and tidal volume contributes to lipopolysaccharide-induced lung injury. Am J Respir Crit Care Med 171:147–157
Doerr CH, Gajic O, Berrios JC, Caples S, Abdel M, Lymp JF, Hubmayr RD (2005) Hypercapnic acidosis impairs plasma membrane wound resealing in ventilator-injured lungs. Am J Respir Crit Care Med 171:1371–1377
Squadrito GL, Pryor WA (1998) Oxidative chemistry of nitric oxide: the roles of superoxide, peroxynitrite, and carbon dioxide. Free Radic Biol Med 25:392–403
Lymar SV, Hurst JK (1996) Carbon dioxide: physiological catalyst for peroxynitrite-mediated cellular damage or cellular protectant? Chem Res Toxicol 9:845–850
Lymar SV, Jiang Q, Hurst JK (1996) Mechanism of carbon dioxide-catalyzed oxidation of tyrosine by peroxynitrite. Biochemistry 35:7855–7861
Briva A, Vadasz I, Lecuona E, Welch LC, Chen J, Dada LA, Trejo HE, Dumasius V, Azzam ZS, Myrianthefs PM, Batlle D, Gruenbaum Y, Sznajder JI (2007) High CO2 levels impair alveolar epithelial function independently of pH. PLoS One 2:e1238
O’Croinin DF, Nichol AD, Hopkins N, Boylan J, O’Brien S, O’Connor C, Laffey JG, McLoughlin P (2008) Sustained hypercapnic acidosis during pulmonary infection increases bacterial load and worsens lung injury. Crit Care Med 36:2128–2135
D’Arcangelo D, Gaetano C, Capogrossi MC (2002) Acidification prevents endothelial cell apoptosis by Axl activation. Circ Res 91:e4–e12
Takeshita K, Suzuki Y, Nishio K, Takeuchi O, Toda K, Kudo H, Miyao N, Ishii M, Sato N, Naoki K, Aoki T, Suzuki K, Hiraoka R, Yamaguchi K (2003) Hypercapnic acidosis attenuates endotoxin-induced nuclear factor-[kappa]B activation. Am J Respir Cell Mol Biol 29:124–132
Coakley RJ, Taggart C, Greene C, McElvaney NG, O’Neill SJ (2002) Ambient pCO2 modulates intracellular pH, intracellular oxidant generation, and interleukin-8 secretion in human neutrophils. J Leukoc Biol 71:603–610
Wang X, Wu J, Li L, Chen F, Wang R, Jiang C (2003) Hypercapnic acidosis activates KATP channels in vascular smooth muscles. Circ Res 92:1225–1232
Laffey JG, Honan D, Hopkins N, Hyvelin JM, Boylan JF, McLoughlin P (2004) Hypercapnic acidosis attenuates endotoxin-induced acute lung injury. Am J Respir Crit Care Med 169:46–56
Rai S, Engelberts D, Laffey JG, Frevert C, Kajikawa O, Martin TR, Post M, Kavanagh BP (2004) Therapeutic hypercapnia is not protective in the in vivo surfactant-depleted rabbit lung. Pediatr Res 55:42–49
Gomes RF, Shen X, Ramchandani R, Tepper RS, Bates JH (2000) Comparative respiratory system mechanics in rodents. J Appl Physiol 89:908–916
Green TP, Johnson DE, Marchessault RP, Gatto CW (1988) Transvascular flux and tissue accrual of Evans blue: effects of endotoxin and histamine. J Lab Clin Med 111:173–183
le Wang F, Patel M, Razavi HM, Weicker S, Joseph MG, McCormack DG, Mehta S (2002) Role of inducible nitric oxide synthase in pulmonary microvascular protein leak in murine sepsis. Am J Respir Crit Care Med 165:1634–1639
Espevik T, Nissen-Meyer J (1986) A highly sensitive cell line, WEHI 164 clone 13, for measuring cytotoxic factor/tumor necrosis factor from human monocytes. J Immunol Methods 95:99–105
Mosmann T (1983) Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65:55–63
Copland IB, Reynaud D, Pace-Asciak C, Post M (2006) Mechanotransduction of stretch-induced prostanoid release by fetal lung epithelial cells. Am J Physiol Lung Cell Mol Physiol 291:L487–L495
Wilson MR, Choudhury S, Goddard ME, O’Dea KP, Nicholson AG, Takata M (2003) High tidal volume ventilation upregulates intrapulmonary cytokines in an in vivo mouse model of ventilator-induced lung injury. J Appl Physiol 95:1385–1393
Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS (1997) Injurious ventilatory strategies increase cytokines and c-fos mRNA expression in an isolated rat lung model. J Clin Invest 99:944–952
von Bethmann AN, Brasch F, Nusing R, Vogt K, Volk HD, Muller KM, Wendel A, Uhlig S (1998) Hyperventilation induces release of cytokines from perfused mouse lung. Am J Respir Crit Care Med 157:263–272
Ricard JD, Dreyfuss D, Saumon G (2001) Production of inflammatory cytokines in ventilator-induced lung injury: a reappraisal. Am J Respir Crit Care Med 163:1176–1180
Bonnans C, Levy BD (2007) Lipid mediators as agonists for the resolution of acute lung inflammation and injury. Am J Respir Cell Mol Biol 36:201–205
Singer CA, Baker KJ, McCaffrey A, AuCoin DP, Dechert MA, Gerthoffer WT (2003) p38 MAPK and NF-kappaB mediate COX-2 expression in human airway myocytes. Am J Physiol Lung Cell Mol Physiol 285:L1087–L1098
Catley MC, Chivers JE, Cambridge LM, Holden N, Slater DM, Staples KJ, Bergmann MW, Loser P, Barnes PJ, Newton R (2003) IL-1beta-dependent activation of NF-kappaB mediates PGE2 release via the expression of cyclooxygenase-2 and microsomal prostaglandin E synthase. FEBS Lett 547:75–79
Mestre JR, Mackrell PJ, Rivadeneira DE, Stapleton PP, Tanabe T, Daly JM (2001) Redundancy in the signaling pathways and promoter elements regulating cyclooxygenase-2 gene expression in endotoxin-treated macrophage/monocytic cells. J Biol Chem 276:3977–3982
Held HD, Boettcher S, Hamann L, Uhlig S (2001) Ventilation-induced chemokine and cytokine release is associated with activation of nuclear factor-kappaB and is blocked by steroids. Am J Respir Crit Care Med 163:711–716
Ricard JD, Dreyfuss D, Saumon G (2002) Ventilator-induced lung injury. Curr Opin Crit Care 8:12–20
Abraham E (2005) Alterations in cell signaling in sepsis. Clin Infect Dis 41(Suppl 7):S459–S464
Minetti M, Mallozzi C, Di Stasi AM (2002) Peroxynitrite activates kinases of the src family and upregulates tyrosine phosphorylation signaling. Free Radic Biol Med 33:744–754
Mallozzi C, Di Stasi AM, Minetti M (2001) Nitrotyrosine mimics phosphotyrosine binding to the SH2 domain of the src family tyrosine kinase lyn. FEBS Lett 503:189–195
Liaudet L, Soriano FG, Szabo C (2000) Biology of nitric oxide signaling. Crit Care Med 28:N37–N52
Ishikawa TO, Jain NK, Taketo MM, Herschman HR (2006) Imaging cyclooxygenase-2 (Cox-2) gene expression in living animals with a luciferase knock-in reporter gene. Mol Imaging Biol 8:171–187
Acknowledgments
Canadian Institutes of Health Research (CIHR). Dr. Kavanagh is the holder of the Dr. Geoffrey Barker Chair in Critical Care Medicine. Dr. Post is the holder of a Canadian Research Chair in Fetal, Neonatal and Maternal Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
V. Peltekova and D. Engelberts contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Figure 1S: Cytokine profile in bronchoalveolar lavage
: Injurious ventilation induced significant elevations in BAL concentrations of interleukin-6 (IL-6, panel A), keratinocyte chemoattractant (KC, panel B) and monocyte chemoattractant protein-1 (MCP-1, Panel C); hypercapnia significantly attenuated all of these cytokine elevations. Data are means ± SD, 4-6 per group. *Injurious ventilation normocapnia vs. all other groups (ANOVA, P < 0.001; Student-Neuman-Keuls test P < 0.05). †Injurious ventilation normocapnia vs. all other groups (ANOVA on ranks, P < 0.001; Dunn’s test, P < 0.01). (PPT 94 kb)
Figure 2S: Adhesion molecule and mediator profile
: Injurious ventilation induced significant elevations in BAL concentrations of matrix metallo-proteinase-9 (MMP-9, panel A), soluble E-selectin (sE-selectin, panel B), and soluble vascular cell adhesion molecule (sV-CAM, panel C); hypercapnia significantly attenuated all of these mediator elevations. Injurious ventilation did not alter the levels of soluble intracellular cell adhesion molecule (iCAM, Panel C). Data are means ± SD, 4-6 per group. *Injurious ventilation normocapnia vs. all other groups (ANOVA, P < 0.001; Student-Neuman-Keuls test P < 0.05). †Injurious ventilation normocapnia vs. all other groups (ANOVA on ranks, P < 0.001; Dunn’s test, P < 0.01). ‡No among-group differences
Figure 3S: Bioactivity of tumor necrosis factor
(alpha): Hypercapnia attenuated both peaks—45 and 180 min—of TNFα activity in lungs of injuriously ventilated mice (panel A). Injurious ventilation resulted in increased levels of TNFα, and hypercapnia attenuated such elevation (panel B). Data are means ± SD, 4-6 per group. *Hypercapnia vs. normocapnia (P < 0.001, two-way ANOVA on ranks; P < 0.05, ANOVA on ranks, normocapnia; P = ns, ANOVA on ranks, hypercapnia; *hypercapnia vs. normocapnia, P < 0.05 Student-Newman-Keuls test). †Injurious ventilation normocapnia vs. all other groups (ANOVA on ranks, P < 0.001; Dunn’s test, P < 0.01)
Figure 4S: Lung tissue eicosanoids
: Stable hydrolysis products of prostaglandins, leukotrienes and lipoxins were measured in lung tissue following injurious ventilation under normocapnic or hypercapnic conditions (liquid chromatography-tandem mass spectrometry, LC-MS/MS). Hypercapnia attenuated the elevation of arachidonic acid (AA), prostaglandin F2α (PGF2α) and thromboxane B2 (TxB2). Data are mean ± SEM, 4–6 per group. *P < 0.05 hypercapnia vs. normocapnia (unpaired t-test)
Rights and permissions
About this article
Cite this article
Peltekova, V., Engelberts, D., Otulakowski, G. et al. Hypercapnic acidosis in ventilator-induced lung injury. Intensive Care Med 36, 869–878 (2010). https://doi.org/10.1007/s00134-010-1787-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1787-7