Abstract
Purpose
To evaluate the plausibility, stability, and interindividual comparability of the global inhomogeneity index (GI) based on electrical impedance tomography (EIT).
Methods
The lung area in an EIT image was identified by using the lung area estimation method, which mirrors the lung regions in the functional EIT image and subsequently subtracts the cardiac-related areas. The tidal EIT image, showing the difference in impedances between end-inspiration and end-expiration, was calculated and the variations in its pixel values within the predefined lung area were then used as an indicator of inhomogeneous ventilation (the GI index). Fifty patients were investigated including 40 patients tracheally intubated with double-lumen tubes (test group) and 10 patients under anesthesia without pulmonary disease (control group). Positive end-expiratory pressure (PEEP) of 5 mbar was applied in the test group during both two-lung ventilation (TLV) and subsequent one-lung ventilation (OLV). The patients of the control group were ventilated without PEEP. EIT data were recorded in both groups.
Results
A significantly lower GI value was found in the control group (0.40 ± 0.05, P = 0.025 vs. TLV 0.74 ± 0.47 and P < 0.002 vs. OLV 1.51 ± 1.45). A significant difference was also found in the test group between TLV and OLV (P < 0.002). If GI was calculated only in the ventilated lung area during OLV (0.71 ± 0.32), it did not significantly differ from the test group during TLV.
Conclusions
The GI index quantifies the gas distribution in the lung with a single number and reveals good interpatient comparability.
Similar content being viewed by others
Introduction
The distribution of the tidal volume in the lungs of patients under mechanical ventilation is often inhomogeneous [1]. Different prevalent conditions may create both collapse of the posterior part and overdistention of the anterior part of the lung, which may increase the risk for ventilator-induced lung injury (VILI) [2]. Ventilation strategies based on information integrated over the whole lung may fail to include inhomogeneity into therapeutical decision-making and thus may not provide optimal therapy [3]. For example, Kunst et al. [4] and Hinz et al. [5, 6] have shown that under static conditions, regional PV curves might considerably differ from the conventional global PV curve. Therefore, it has been suggested that regional inhomogeneities in the damaged lung be taken into consideration to develop improved ventilation strategies [7].
Other methods such as computed tomography (CT), which has a very good spatial resolution [8], and the multibreath washout technique, which has a good temporal resolution [9, 10], are able to detect the inhomogeneous distribution of tidal volume in the lung. However, these methods are not suitable for bedside monitoring.
Electrical impedance tomography (EIT) is a noninvasive, radiation-free imaging technique that can be used at the bedside for monitoring the regional lung ventilation and tidal volume distribution. EIT measures the electrical potentials at the chest wall surface based on the phenomenon that changes in regional air content and regional blood flow modify the electrical impedance of lung tissue [11, 12]. The reliability of EIT has already been confirmed by comparison with different conventional methods, such as CT [13], single photon emission computer tomography [14], and pneumotachography [15]. However, EIT provides complex information on regional ventilation that is difficult to interpret [3, 16]. In addition, the EIT images obtained from different patients can not be compared directly, since they only display relative impedance values. Thus, we have recently developed a global inhomogeneity index (GI) to quantify the tidal volume distribution within the lung [17]. The tidal EIT image, showing the difference in impedances between end-inspiration and end-expiration, was first calculated and the variations in its pixel values were then used as an indicator of inhomogeneous ventilation.
The aim of this study was to evaluate the stability and comparability of the GI index in a clinical setting. Recently, it has been shown that EIT can be used to confirm the placement of double-lumen tube (DLT) [18]. Therefore, the first hypothesis of our study was that the GI index should be able to clearly indicate the difference between the tidal volume distributions during one-lung ventilation (OLV) and two-lung ventilation (TLV). Our second hypothesis was that GI should also be able to differentiate between the tidal volume distributions in healthy and diseased lungs. Consequently, patients with healthy lungs were included in our study and served as a control group.
Materials and methods
Fifty patients were studied and divided into two groups. Ten sedated patients (control group) with healthy lungs [ASA I or ASA II; 7 male, 3 female; age 30 ± 10 years; height 179 ± 8 cm; weight 77 ± 9 kg (mean ± SD)] were mechanically ventilated in the volume-controlled mode for orthopedic surgery. Forty patients (test group: ASA I–III; 28 male, 12 female; age 66 ± 13 years; height 171 ± 8 cm; body weight 75 ± 13 kg) were tracheally intubated with DLT, and subsequently OLV for thoracic surgical procedures was performed [18]. Exclusion criteria included age <18 years, pregnancy and lactation period, and any contraindication for the use of EIT (pacemaker, automatic implantable cardioverter defibrillator, and implantable pumps). An additional exclusion criterion for the control group was history or clinical signs of lung disease. The study was approved by the local ethics committee. Written informed consent was obtained from all patients prior to the study.
Protocol for the control group
Anesthesia was induced by bolus injection of propofol and fentanyl and was maintained by continuous infusion of propofol. Following muscle relaxation (vecuronium bromide), tracheal intubation (tube ID 7.0 for women and 8.0 for men) was performed. The patients were mechanically ventilated in volume-controlled mode (10 ml/kg body weight, ventilatory frequency 12 min−1, I:E 1:1.5, FIO2 1.0, PEEP 0 mbar) using Evita4Lab (Dräger Medical, Lübeck, Germany). All patients remained in the supine position, and no surgical procedure was started before the protocol was accomplished.
Electrical impedance tomography measurement was performed before the surgical procedure.
Protocol for test group
The protocol applied in the patients of the test group is described in detail in [18] and is given here in short. After induction of anesthesia and achievement of complete muscle relaxation, the trachea was intubated with a left-sided DLT (Broncho-Cath, Mallinckrodt, Athlone, Ireland) of appropriate size. After tracheal intubation, both lungs were mechanically ventilated (Cicero EM, Dräger Medical, Lübeck, Germany) in volume-controlled mode (10 ml/kg body weight, ventilatory frequency 12 min−1, FIO2 1.0, PEEP 5 mbar). During OLV, the tidal volume was reduced to 5 ml/kg body weight.
Electrical impedance tomography measurement was performed during TLV after endotracheal placement of the DLT and during left and right OLV in the supine position.
EIT data collection and analysis
An EIT electrode belt, which carries 16 electrodes with a width of 40 mm, was placed around the thorax in the fifth intercostal space, and one reference electrode was placed at the patients’ abdomen (EIT Evaluation KIT 2, Dräger Medical, Lübeck, Germany). EIT images were continuously recorded at 20 Hz and stored. The EIT electrode belt was removed before surgery.
For the control group, an EIT video sequence of 5-min duration including about 60 breathing cycles from every patient was analyzed. Also for the test group, during TLV, EIT video sequences of 5-min duration were taken for analysis; during OLV, 12 breathing cycles from each patient were analyzed. The GI index was calculated from the analyzed data for every breathing cycle.
The calculation of GI
The GI index was recently introduced by our group [17]. While that paper introduced different indices and their combination to titrate PEEP based on EIT imaging, here we focus exclusively on the GI index. In short the GI is calculated in the following way: For every breathing cycle, a so-called tidal image is first generated. Each pixel of these tidal images represents the difference in impedance between end-inspiration and end-expiration. The median value of each tidal image is calculated for the lung area. The sum of the absolute difference between median value and every pixel value is considered to indicate the variation in the tidal volume distribution in the whole lung region. In order to make the GI index universal and interpatient comparable, it is normalized to the sum of the impedance values within the lung area:
where DI denotes the value of the differential impedance in the tidal images, DI xy is the pixel in the identified lung area, and DIlung is all the pixels representing the lung area.
The identification of the lung area is a prerequisite for the GI calculation. We recently proposed a novel method for lung area estimation (LAE) [19]. In brief, it is based on those lung regions that are determined by functional EIT (fEIT) with a predefined threshold [20]. These regions were mirrored and the cardiac-related areas were subtracted. The details of our LAE method are given in the electronic supplementary material.
Evaluation of GI
Air distribution between left and right lungs during tidal ventilation was evaluated by the ratioL,R/TV calculated as follows: the relative impedance values in the EIT images in the most ventilated lung are divided by that of both lungs. This ratio is normalized with the number of pixels in the predefined lung area. Ideally, ratioL,R/TV should be 0.5 for healthy people and 1 if only one lung is ventilated.
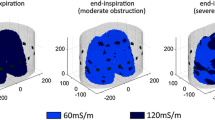
Using the EIT data obtained during OLV, we calculated the GI in two different ways: (i) GI from the ventilated lung only [OLV(i)], and (ii) GI from ventilated and nonventilated lung [OLV(ii)] (Fig. 1). The results were compared to those calculated in patients from the control group (healthy) and from the test group during TLV.
Illustration of GI calculation in three different situations. Left During TLV, GI calculated from both lungs. Middle During OLV, situation i [OLV(i)], GI calculated from the ventilated lung. Right Situation ii [OLV(ii)], GI calculated from both lungs. The same lung area determined during TLV with the LAE method was used for TLV and OLV(ii). The fEIT method was used during OLV for OLV(i)
The influence of threshold value of the fEIT method (the first step of LAE method) on the GI calculation was evaluated. Threshold values from 0–60% were used and the corresponding GIs were calculated, respectively.
Statistical analysis
Statistical analysis was performed using the one-way ANOVA (MATLAB 7.2 statistic toolbox, The MathWorks, Natick, MA, USA). Results were compared using the Bland–Altman analysis [21]. A P-value <0.05 was considered statistically significant. Data are presented as mean and standard deviation (SD).
Results
RatioL,R/TV was 0.52 ± 0.01 for control group, 0.60 ± 0.11 for test group during TLV, and 0.87 ± 0.07 during OLV. A value close to 0.5 does not necessarily mean a homogeneous air distribution in the whole respiratory system, but a value close to 1 definitely means inhomogeneous distribution between the left and right lungs according to EIT data. There were five patients in test group during TLV with ratioL,R/TV > 0.75 and the maximum was 0.87.
Table 1 shows the GI of every patient of the control group and of the test group during TLV. Due to technical problems during the measurement, three patients (test group) were excluded from the analysis. The GI index seemed stable since the standard deviations of GI as taken from about 60 breathing cycles (5-min EIT video sequence) in each patient of both the control and test groups were considerably low.
The boxplot in Fig. 2 shows the comparison of GI calculated from the control group data, TLV data, OLV(i), and OLV(ii). The mean GI value of each patient was used for comparison. There are significant differences between control group and TLV (P = 0.025), TLV and OLV(ii) (P < 0.002), OLV(i) and OLV(ii) (P < 0.002), and between control group and OLV(ii) (P < 0.002). No difference was found between TLV and OLV(i) (see also Fig. 3).
GI of control group (healthy) and test group [TLV, OLV(i), OLV(ii)]. TLV GI from two-lung ventilation, OLV (i) GI from the ventilated lung only during one-lung ventilation (OLV), OLV (ii) GI from ventilated and nonventilated lung during one-lung ventilation. The boxes mark the quartiles while the whiskers extend from the box out to the most extreme data value within 1.5× the interquartile range of the sample. *P = 0.025, significantly different from the control group; **P < 0.002, significantly different from the control group, from the test group itself during TLV, and from OLV(i)
Bland–Altman plot to compare the GI values during TLV and OLV(i) (left), TLV and OLV(ii) (right). Each circle represents one patient from the test group. Dashed line in the middle depicts the mean value of the whole data set. The other two dashed lines represent one standard deviation. The red asterisk shows the extreme case where ventilation distribution in the lung during TLV was worse than that during OLV(ii)
The differences between GI during TLV and OLV(i), as well as during TLV and OLV(ii) using Bland–Altman analysis revealed that the GI values were similar during TLV and OLV(i) (Fig. 3, left) but differed during TLV and OLV(ii) for every individual (Fig. 3, right).
Figure 4 illustrates the influence of threshold value (the threshold used in the fEIT method, the first step of the LAE method) on GI calculation in one patient from the control group. The GI value decreased while the threshold value increased. Similar results were found in other patients from both the control and test groups.
Discussion
As the main result of the present study, we found it feasible to quantify a complex differential (end-inspiration minus end-expiration) pulmonary impedance pattern derived from EIT imaging in one number, the GI index. A recent study demonstrated the predictive power of GI for setting PEEP [17]. However, there was no proof that GI was interpatient comparable. Although no reference method was used (e.g., CT), we evaluated our GI clinically by comparing the GI values calculated from the TLV data with those derived from the OLV data. Since the patients scheduled for thoracic surgical procedures may have severe lung diseases, in extreme cases, ventilation distribution in the lung during TLV may have deteriorated to a similar or even larger degree as during OLV(ii) (asterisk in Fig. 3 and ratioL,R/TV) due to the difference in ventilator settings (10 vs. 5 ml/kg body weight). This may also explain the overlap of the box plot in Fig. 2 between TLV and OLV(ii). But after all, as hypothesized, we found GI to be significantly higher for OLV(ii) compared to OLV(i) and TLV, and to be similar for OLV(i) and TLV (Figs. 2, 3). We also found significant differences in GI between healthy lungs and damaged lungs (Fig. 2). These findings give indirect proof of the reliability and interindividual comparability of GI. Small variations in the results (see the SD values in Table 1) also prove that the GI values are stable within every individual.
The standard ventilator settings for patients receiving only short-term ventilation during surgery (FIO2 1.0 and 10 ml/kg) were applied [22]. Notice that the participants in the control group were sedated and ventilated with zero end-expiratory pressure (ZEEP). The patients in the test group were ventilated with a PEEP of 5 mbar. Under condition of anesthesia, the alveoli in the dependent lung may collapse, which may lead to an inhomogeneous air distribution in the entire lung [23, 24]. However, with respect to ventilation homogeneity, the state of the lung seems more important compared to the PEEP effect, i.e. the air distribution in the healthy lung is more homogeneous compared to the diseased lung with a low PEEP.
There have already been many studies on the inhomogeneity of the air distribution in the lung based on EIT analysis [2, 4, 5, 25–29]. Frerichs et al. [26] calculated a weighted mean “geometrical centre” of ventilation to quantify the changes in ventilation distribution occurring in the dorsal-to-ventral direction. Further, fractional ventilation was determined in 64 ROIs in the left and right halves of the scans (32 ROIs in each half) [29]. Kunst et al. [27] divided the EIT image into anterior and posterior parts of the lung region and calculated an “impedance ratio,” i.e., the ratio between the ventilation-induced impedance changes in these two parts of the lung. Victorino et al. [2] compared the regional ventilation in different ROIs with EIT and CT. However, these attempts to depict the inhomogeneity by comparison between simple geometric ROIs have their limitation. Only the ratios, i.e., left side to the right side, anterior part to posterior part, were analyzed, whereas the impedance pattern associated with each ROI is not described by these methods. In the worst case, the air could be equally distributed among different ROIs but distribution can be strongly inhomogeneous within certain ROIs.
Meier et al. [25] took a step forward insofar as they divided the tidal volume change into the tidal volume gain and loss. In this way, the authors tried to detect inhomogeneous changes in the regional distribution of tidal volume. However, this method would add more information than the other methods only if the tidal volume changed during the ventilation process. Hinz et al. [5] analyzed the regional PV curves for every pixel in the regions defined as the “EIT lung region.” Up to 912 regional PV curves might be reconstructed in the whole image. Of course much more information will be gained, but at the same time the method is not applicable for clinical use. Pulletz et al. [28] analyzed the tidal volume distribution based on fEIT and two other types of ROI definition but again divided the EIT scans into left and right regions. The GI, as one compact index, contains information taken from every pixel of the lung area in the EIT image and is able to describe the inhomogeneity of tidal volume distribution in the entire lung.
One limitation of the GI is that it does not consider the local distribution effect. Although it is good enough for the current patient data set, it might be improved by adding the LI, which was also developed by our group and presented earlier [17]. The LI calculates the differences among the pixels and their neighbor pixels. These two indices, GI and LI, emphasize different aspects of inhomogeneity of the air distribution, therefore it may be reasonable to combine them in order to find a suitable ventilation strategy. Since both indices are normalized, they can be combined simply by multiplication [17].
Another limitation is that the GI value differs when different lung area determination methods are used. For a given patient, the size of the lung area may differ considerably based on the method used for its determination. Both the early suggested method by Hahn and Frerichs [26, 30, 31] and the method modified by Hinz [5] may fail to detect parts of the lung regions in the EIT images when some lung diseases exist. Pulletz et al. [32] recommended combining the fEIT and simple geometric ROIs for lung function analysis in certain pathological situations. This was not applicable however for GI calculation. Therefore, the mirrored lung regions without cardiac-related areas (the LAE method) are used to calculate the GI. The advantages and limitations of the LAE method are discussed in the electronic supplementary material by comparing LAE with the method of Hahn et al. [33].
As shown by Pulletz et al. [32], different threshold values in the fEIT method lead to different sizes of lung area. Using fEIT method as the first step, the LAE method would deliver different results and thus the GI value would be influenced (Fig. 4). It was previously suggested that a threshold between 20 and 35% should be used [32]. In our GI calculation, 20% was applied. Different threshold values may be applied, but they should be used consistently so that the corresponding GI values are interpatient comparable.
The GI index may be further used in other diseases that are associated with inhomogeneous tidal volume distribution in the lung such as pneumothorax, acute respiratory distress syndrome (ARDS), and asthmatic bronchitis. Costa et al. [34] suggested a method to detect pneumothorax using EIT. However, their method cannot be used for diagnosing stable preexisting pneumothoraces [34]. Absolute EIT technique seems promising in detecting pneumothorax [35]. Artifacts in outer regions, systematic errors and differences in absolute values of tissue resistivity among individuals and trials indicate that further development is needed for this technique however. Since our GI enables interpatient comparison, it may be possible to set up a threshold that may be used to distinguish healthy patients from pneumothorax patients. However, further investigation is necessary to evaluate GI for its predictive value.
Conclusions
The GI index has proved to be reliable and interpatient comparable. It is able to depict the tidal volume distribution in the lung with respect to the disease state of the lung and to the ventilation pattern. Thus, it may prove to be a useful tool to guide ventilation therapy.
References
Gattinoni L, D’Andrea L, Pelosi P, Vitale G, Pesenti A, Fumagalli R (1993) Regional effects and mechanism of positive end-expiratory pressure in early adult respiratory distress syndrome. JAMA 269:2122–2127
Victorino JA, Borges JB, Okamoto VN, Matos GF, Tucci MR, Caramez MP, Tanaka H, Sipmann FS, Santos DC, Barbas CS, Carvalho CR, Amato MB (2004) Imbalances in regional lung ventilation: a validation study on electrical impedance tomography. Am J Respir Crit Care Med 169:791–800
Putensen C, Wrigge H, Zinserling J (2007) Electrical impedance tomography guided ventilation therapy. Curr Opin Crit Care 13:344–350
Kunst PW, Bohm SH, Vazquez de Anda G, Amato MB, Lachmann B, Postmus PE, de Vries PM (2000) Regional pressure volume curves by electrical impedance tomography in a model of acute lung injury. Crit Care Med 28:178–183
Hinz J, Moerer O, Neumann P, Dudykevych T, Frerichs I, Hellige G, Quintel M (2006) Regional pulmonary pressure volume curves in mechanically ventilated patients with acute respiratory failure measured by electrical impedance tomography. Acta Anaesthesiol Scand 50:331–339
Hinz J, Gehoff A, Moerer O, Frerichs I, Hahn G, Hellige G, Quintel M (2007) Regional filling characteristics of the lungs in mechanically ventilated patients with acute lung injury. Eur J Anaesthesiol 24:414–424
Rouby JJ, Lu Q, Goldstein I (2002) Selecting the right level of positive end-expiratory pressure in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 165:1182–1186
Gattinoni L, Caironi P, Valenza F, Carlesso E (2006) The role of CT-scan studies for the diagnosis and therapy of acute respiratory distress syndrome. Clin Chest Med 27:559–570 (abstract vii)
Schibler A, Henning R (2002) Positive end-expiratory pressure and ventilation inhomogeneity in mechanically ventilated children. Pediatr Crit Care Med 3:124–128
Schmalisch G, Proquitte H, Roehr CC, Wauer RR (2006) The effect of changing ventilator settings on indices of ventilation inhomogeneity in small ventilated lungs. BMC Pulm Med 6:20
Nopp P, Rapp E, Pfutzner H, Nakesch H, Ruhsam C (1993) Dielectric properties of lung tissue as a function of air content. Phys Med Biol 38:699–716
Brown BH, Barber DC, Morice AH, Leathard AD (1994) Cardiac and respiratory related electrical impedance changes in the human thorax. IEEE Trans Biomed Eng 41:729–734
Frerichs I, Hinz J, Herrmann P, Weisser G, Hahn G, Dudykevych T, Quintel M, Hellige G (2002) Detection of local lung air content by electrical impedance tomography compared with electron beam CT. J Appl Physiol 93:660–666
Hinz J, Neumann P, Dudykevych T, Andersson LG, Wrigge H, Burchardi H, Hedenstierna G (2003) Regional ventilation by electrical impedance tomography: a comparison with ventilation scintigraphy in pigs. Chest 124:314–322
Marquis F, Coulombe N, Costa R, Gagnon H, Guardo R, Skrobik Y (2006) Electrical impedance tomography’s correlation to lung volume is not influenced by anthropometric parameters. J Clin Monit Comput 20:201–207
Wolf GK, Arnold JH (2006) Electrical impedance tomography: ready for prime time? Intensive Care Med 32:1290–1292
Zhao Z, Möller K, Steinmann D, Guttmann J (2008) Global and local inhomogeneity indices of lung ventilation based on electrical impedance tomography. In: Vander Sloten J, Verdonck P, Nyssen M, Haueisen J (eds) ECIFMBE 2008, IFMBE Proceedings 22. Springer, Berlin, pp 256–259
Steinmann D, Stahl CA, Minner J, Schumann S, Loop T, Kirschbaum A, Priebe HJ, Guttmann J (2008) Electrical impedance tomography to confirm correct placement of double-lumen tube: a feasibility study. Br J Anaesth 101:411–418
Zhao Z, Möller K, Steinmann D, Guttmann J (2009) Determination of lung area in EIT images. In: Proceedings of the 3rd conference on iCBBE, Beijing, China. IEEE (in press)
Hahn G, Sipinkova I, Baisch F, Hellige G (1995) Changes in the thoracic impedance distribution under different ventilatory conditions. Physiol Meas 16:A161–A173
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Putensen C, Wrigge H (2007) Tidal volumes in patients with normal lungs: one for all or the less, the better? Anesthesiol 106:1085–1087
Tusman G, Bohm SH, Suarez-Sipmann F, Turchetto E (2004) Alveolar recruitment improves ventilatory efficiency of the lungs during anesthesia. Can J Anaesth 51:723–727
Hedenstierna G, Edmark L (2005) The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 31:1327–1335
Meier T, Luepschen H, Karsten J, Leibecke T, Grossherr M, Gehring H, Leonhardt S (2008) Assessment of regional lung recruitment and derecruitment during a PEEP trial based on electrical impedance tomography. Intensive Care Med 34:543–550
Frerichs I, Hahn G, Golisch W, Kurpitz M, Burchardi H, Hellige G (1998) Monitoring perioperative changes in distribution of pulmonary ventilation by functional electrical impedance tomography. Acta Anaesthesiol Scand 42:721–726
Kunst PW, Vazquez de Anda G, Bohm SH, Faes TJ, Lachmann B, Postmus PE, de Vries PM (2000) Monitoring of recruitment and derecruitment by electrical impedance tomography in a model of acute lung injury. Crit Care Med 28:3891–3895
Pulletz S, Elke G, Zick G, Schadler D, Scholz J, Weiler N, Frerichs I (2008) Performance of electrical impedance tomography in detecting regional tidal volumes during one-lung ventilation. Acta Anaesthesiol Scand 52:1131–1139
Frerichs I, Dargaville PA, van Genderingen H, Morel DR, Rimensberger PC (2006) Lung volume recruitment after surfactant administration modifies spatial distribution of ventilation. Am J Respir Crit Care Med 174:772–779
Frerichs I, Hahn G, Schroder T, Hellige G (1998) Electrical impedance tomography in monitoring experimental lung injury. Intensive Care Med 24:829–836
Hahn G, Frerichs I, Kleyer M, Hellige G (1996) Local mechanics of the lung tissue determined by functional EIT. Physiol Meas 17(Suppl 4A):A159–A166
Pulletz S, van Genderingen HR, Schmitz G, Zick G, Schadler D, Scholz J, Weiler N, Frerichs I (2006) Comparison of different methods to define regions of interest for evaluation of regional lung ventilation by EIT. Physiol Meas 27:115–127
Hahn G, Dittmar J, Just A, Hellige G (2008) Improvements in the image quality of ventilatory tomograms by electrical impedance tomography. Physiol Meas 29:S51–S61
Costa EL, Chaves CN, Gomes S, Beraldo MA, Volpe MS, Tucci MR, Schettino IA, Bohm SH, Carvalho CR, Tanaka H, Lima RG, Amato MB (2008) Real-time detection of pneumothorax using electrical impedance tomography. Crit Care Med 36:1230–1238
Hahn G, Just A, Dudykevych T, Frerichs I, Hinz J, Quintel M, Hellige G (2006) Imaging pathologic pulmonary air and fluid accumulation by functional and absolute EIT. Physiol Meas 27:S187–S198
Acknowledgements
This work was partially supported by the Deutsche Forschungsgemeinschaft (Grant #GU 561/6-1) and by Bundesministerium für Bildung und Forschung (Grant 1781X08 MOTiF-A).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhao, Z., Möller, K., Steinmann, D. et al. Evaluation of an electrical impedance tomography-based global inhomogeneity index for pulmonary ventilation distribution. Intensive Care Med 35, 1900–1906 (2009). https://doi.org/10.1007/s00134-009-1589-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1589-y