Abstract
Objective
The aim of our study was to determine the effect of the irregular spontaneous breathing pattern and posture on the spatial distribution of ventilation in neonates free from respiratory disease by the non-invasive imaging method of electrical impedance tomography (EIT). Scanning of spontaneously breathing neonates is the prerequisite for later routine application of EIT in babies with lung pathology undergoing ventilator therapy.
Design
Prospective study.
Setting
Neonatal intensive care unit at a university hospital.
Patients
Twelve pre-term and term neonates (mean age: 23 days; mean body weight: 2,465 g; mean gestational age: 34 weeks; mean birth weight: 2,040 g).
Interventions
Change in body position in the sequence: supine, right lateral, prone, supine.
Measurements and results
EIT measurements were performed using the Göttingen GoeMF I system. EIT scans of regional lung ventilation showing the distribution of respired air in the chest cross-section were generated during phases of rapid tidal breathing and deep breaths. During tidal breathing, 54.5±8.3%, 55.2±10.5%, 59.9±8.4% and 54.2±8.5% of inspired air (mean values ± SD) were directed into the right lung in the supine, right lateral, prone and repeated supine postures respectively. During deep inspirations, the right lung ventilation accounted for 52.6±7.9%, 68.5±8.5%, 55.4±8.2% and 50.5±6.6% of total ventilation respectively.
Conclusion
The study identified the significant effect of breathing pattern and posture on the spatial distribution of lung ventilation in spontaneously breathing neonates. The results demonstrate that changes in regional ventilation can easily be determined by EIT and bode well for the future use of this method in paediatric intensive care.
Similar content being viewed by others
Introduction
Electrical impedance tomography (EIT) is a relatively new non-invasive radiation-free imaging method providing cross-sectional scans of the body on the basis of the measurement of electrical tissue properties. In recent years, intensivists have shown an increasing interest in this method. There are three major reasons explaining the growing attractiveness of EIT for clinicians:
-
1.
Electrical impedance tomography measures a new tissue quality that is not being addressed by other established examination tools. Access to such a novel form of information may increase the clinical diagnostic and monitoring possibilities of identifying structural and functional tissue and organ changes
-
2.
The method exhibits several advantages over other imaging techniques. Electrical impedance tomography allows frequent examinations at scan rates approaching several tens of scans per second, which can be performed at the bedside as no radiation is used
-
3.
Technological developments have decidedly improved the performance of modern EIT devices [1], which now enable stable and undisturbed measurements even in an electrically noisy environment, e.g. in intensive care units (ICU)
Monitoring of regional lung ventilation is the most promising application of EIT in intensive care [2]. Electrical properties of the lung tissue are significantly influenced by air content and several experimental validation studies using electron beam computed tomography [3], ventilation scintigraphy [4] and staining techniques [5] have documented the ability of adequate EIT technology to identify local changes in lung air volume. Thanks to the excellent time resolution EIT is able to determine not only the local magnitude of lung ventilation and local resting volume (e.g. [6, 7]) but also the dynamics of local filling and emptying of lung units [8]. In view of these EIT features in monitoring local lung function, it is expected that EIT may be useful in the assessment of the efficacy of therapeutic interventions, including mechanical ventilation, and in the prediction of the progress of acute and chronic lung disease.
Critically ill neonates may particularly benefit from the use of this new technique. In addition to the advantages of EIT application already mentioned, this patient group may profit significantly from the reduction in required radiographic examinations. Our recent study performed on mechanically ventilated critically ill infants [9] indicated that EIT was able to determine changes in local lung ventilation in response to adjusted ventilator settings, surfactant instillation and postural changes. However, at the same time it became evident that in order to make conclusions regarding the effect of mechanical ventilation on regional lung ventilation in neonates and small infants suffering from lung disease it is essential to know how lung ventilation is distributed under normal physiological conditions and during spontaneous breathing. In the group of pre-term and term neonates, this information is lacking, because, for ethical reasons, there exists no justification for the application of invasive methods to study regional lung ventilation in otherwise healthy neonates, and, furthermore, the available examination techniques are not applicable without the disturbance of the spontaneous breathing pattern.
Thus, the aim of our study was to examine regional lung ventilation in spontaneously breathing neonates free of any clinical respiratory disorder using advanced EIT technology, and to determine the effect of the irregular spontaneous breathing pattern and body position on the spatial distribution of lung ventilation.
Materials and methods
Patients
Twelve unsedated, spontaneously breathing newborn infants, of whom 10 were pre-term, were studied. The study was approved by the university ethics committee and informed written consent was obtained from the parents. The measurements were conducted according to the principles of Helsinki. Basic characteristics of the patient group are given in Table 1.
The infants were studied either on the day of or one day before their discharge from hospital. Most of the neonates studied were treated in the ICU because of their immaturity. The two term newborns were transferred to the ICU because of hypoxic episodes of unclear origin at birth, which, however, disappeared in the postpartum period. Bacterial infection was suspected with temporarily increased plasma levels of inflammation markers. All infants were free of any manifest respiratory disorder. None of them required either invasive or non-invasive mechanical ventilation.
Electrical impedance tomography
The principle of EIT is based on rapid cyclic acquisition of potential differences on the surface of the chest resulting from repetitive injections of small alternating electrical currents. Both the voltage measurements and current injections take place between pairs of conventional self-adhesive surface electrodes of a 16-electrode array attached on the chest circumference. Electrical impedance tomography scans are generated from the collected potential differences and the known excitation currents using weighted back-projection (see, e.g. [10]) in a 32×32 pixel matrix. Each pixel of the scan shows the instantaneous local relative impedance change with respect to a reference state of local impedance. Further details on EIT basics can be found in multiple publications (e.g. [2, 11, 12]). Electrical impedance tomography scans are circular with the following orientation: the ventral area is at the top and the right side of the body is on the left of the image.
In our study, EIT measurements were carried out using the Göttingen high-performance EIT tomograph GoeMF I [1], operating with excitation currents of 5 mArms and 50 kHz. The acquisition of EIT scans was performed periodically. During each scanning period, 1,000 scans were acquired at a rate of 25 scans per second.
Protocol
All neonates were studied immediately after having been fed. The examination lasted approximately 50 to 60 min. At first, 16 ECG electrodes (Blue Sensor BR-50-K, Medicotest A/S, Ølstykke, Denmark) were applied on the chest circumference and connected to the EIT device. The newborns were positioned in the supine posture and after a few minutes they usually fell asleep. Thereafter, the first EIT data were acquired during two to three scanning periods. The posture was then changed to right lateral, then to prone with the head rotated to one side and finally back to the supine position. In each body position, EIT scanning was repeatedly performed during two to three separate scanning periods.
Off-line data analysis
The respiratory breathing pattern of pre-term but also term newborns is irregular [13, 14]. Often, periodic breathing with respiratory and even apnoeic pauses is observed. The aim of our study was to determine the magnitude and distribution of local lung ventilation and the irregularity of the neonatal breathing pattern gave us the opportunity to quantitatively characterise these parameters during two characteristic periods of breathing:
-
1.
Stable, low tidal volume (VT) breathing at rapid respiratory rates
-
2.
Spontaneous large inspirations, typically occurring in the form of sighs
Therefore, the initial step in the off-line data analysis was the isolation of sequences of EIT scans from the original long series of 1,000 scans that were collected during such periods of tidal breathing and deep inspiration. The following criteria for the selection of tidal breathing phases were used:
-
1.
Duration of more than five breaths
-
2.
Regular breathing rate >50·min–1
-
3.
Stable tidal volume and end-expiratory lung volume
-
4.
Rejection of the first breath if a respiratory pause preceded the tidal breathing period
In each posture, the EIT data from one tidal breathing period and one deep breath were used for quantitative evaluation and generation of derived functional EIT images. Usually, the irregularity of the breathing pattern did not allow repetitive identification of such phases.
In the next data evaluation step, the magnitude of the local air volume changes occurring during tidal or deep breaths was quantified using the following procedure. At first, the end-expiratory and end-inspiratory data points were identified in the selected series of EIT data obtained during tidal breathing. The individual breath-by-breath differences between the corresponding values were then calculated in each pixel of the EIT chest scans and, afterwards, the local average tidal end-expiratory-to-end-inspiratory relative impedance changes were determined from all breaths analysed. Local end-expiratory-to-end-inspiratory relative impedance changes were also calculated during deep inspirations by subtracting the minimum from the maximum value of relative impedance change in the selected series of EIT data (see Fig. 1, top). Thereafter, new EIT images, showing the cross-sectional distribution of the calculated local end-expiratory-to-end-inspiratory relative impedance changes using a grey tone scale, were generated from each tidal breathing and deep breath period (Fig. 1, bottom). The lighter an area, the larger the local end-expiratory-to-end-inspiratory relative impedance change. These images were previously termed by us "functional EIT images of regional lung ventilation" [6, 8]. They characterise the magnitude of local ventilation in the chest cross-section and visualise the ventilated lung regions. Finally, the sum of all pixel values of end-expiratory-to-end-inspiratory relative impedance change, lying within the right and left lung regions, was calculated. This quantitative parameter was used to determine the fractional distribution of ventilation between the right and left lung regions in different postures.
Electrical impedance tomography (EIT) measurement in infant 9 in the supine posture. The tracing of relative impedance change (top) shows the average data in the chest cross-section. The large impedance fluctuations are related to ventilation and reflect the changes in pulmonary air content; the small ones, discernible during respiratory pauses, are related to cardiac action and lung perfusion and occur at a frequency corresponding to the heart rate. The enhanced parts of the tracing show those sections of the measurement that were used to determine the magnitude of local end-expiratory-to-end-inspiratory impedance change during tidal breathing and deep inspiration, and to generate functional EIT images of regional lung ventilation. The arrows show the average difference between the end-expiratory and end-inspiratory data points. The EIT images clearly visualise the lower air volume changes occurring during tidal breathing compared with the large breath. The larger the local air volume change, the lighter the area in the functional EIT image appears to be
The results in the text and figures are presented as mean values ± SD. The statistical analysis was performed using the Student's paired t-test. P values <0.05 were considered significant. In case of multiple comparisons, adjusted significance values were applied according to the classical Bonferroni test.
Results
All neonates studied exhibited a high irregularity of their breathing pattern. Periodic breathing was observed in all subjects. Although respiratory pauses were frequent, no apnoeic phases (i.e. respiratory pauses >10 s) were observed. The selected periods of stable, rapid tidal breathing spanned 5–11 consecutive breaths. The mean number of breaths analysed was 6.8±2.0, 6.3±1.2, 7.3±1.6 and 6.0±1.7 in the supine, right lateral, prone and supine positions respectively. During the selected tidal breathing phases, the mean respiratory rate was 70.6±12.7·min–1, 68.3±16.2·min–1, 70.3±11.1·min–1 and 67.5±9.3·min–1 in the supine, right lateral, prone and repeated supine postures respectively. The average breathing rate over longer time intervals, comprising not only the phases of rapid breathing but also respiratory pauses and sighs, was naturally lower. Neither the number of respiratory cycles selected nor the breathing rate significantly differed with regard to posture.
The generated EIT images of regional lung ventilation showed the distribution of lung ventilation in the chest cross-section. Exemplary images obtained in one neonate (infant 2) during periods of rapid tidal breathing and deep inspiration in all postures studied are presented in Fig. 2. Deep inspirations caused no striking differences in the distribution of ventilation in this neonate from that seen during tidal breathing, either in the initial or final observations made in the supine posture. However, in the right lateral position, the right, dependent lung was less ventilated than the left, non-dependent one during tidal breathing, whereas the opposite was true during deep inspiration. In the prone position, an apparent inhomogeneity of ventilation distribution with pronounced ventilation of the right lung was discernible during tidal breathing, which, however, was not present during deep inspiration.
Functional EIT images of regional lung ventilation obtained in infant 2 in different body positions during rapid tidal breathing and deep inspirations. The images originating from tidal breathing periods (top) are all scaled to the same maximum value of end-expiratory-to-end-inspiratory relative impedance change during this form of breathing. The scale of the images showing deep breaths (bottom) is larger. It corresponds to the maximum value of end-expiratory-to-end-inspiratory relative impedance change during large spontaneous inspirations. This approach is more suitable for a visual comparison of ventilation distributions during tidal breathing and deep inspirations than if a single scale were used
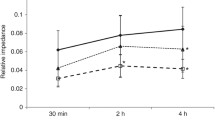
The quantitative results are shown in Figs. 3 and 4. During rapid tidal breathing, the sum of end-expiratory-to-end-inspiratory relative impedance changes, representative of the magnitude of ventilation in the right and left lung regions, was significantly reduced in both lungs in the right lateral posture and in the left lung region in the prone posture when compared with the initial supine posture (Fig. 3). This parameter exhibited a significant difference between the right and left lung regions in the prone position. During deep inspirations, a significant increase of the sum of end-expiratory-to-end-inspiratory relative impedance changes in the right lung region was revealed in the right lateral posture in comparison with the first supine data, whereas a decrease was observed in the left lung region (Fig. 4). The data obtained during the initial and final supine postures did not significantly differ from each other either during tidal breathing or deep inspirations.
Sum of local end-expiratory-to-end-inspiratory relative impedance changes in the right and left lung regions during deep inspirations. To visualise the much larger magnitude of these data in comparison with rapid tidal breathing, fine dotted lines in the lower part of the diagram show the tidal breathing data presented in Fig. 3
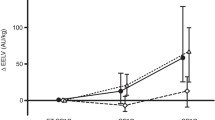
Figure 5 (left) shows the contribution of the right and left lung to the calculated overall sum of end-expiratory-to-end-inspiratory relative impedance changes during rapid tidal breathing and deep inspiration. This form of data presentation also revealed the small, but significantly higher ventilation of the right lung during tidal breathing in the prone posture, as well as the highly significant (P<0.01) difference in ventilation of the right and left lung regions during deep inspirations in the right lateral posture. Figure 5 (right) shows the relative area of the right and left lung regions by end-inspiration during tidal breathing and deep inspirations in all postures studied. The most striking difference in favour of the right lung was found during deep inspiration in the right lateral position.
Discussion
In our study, regional lung ventilation was studied in spontaneously breathing healthy neonates by the non-invasive radiation-free imaging technique of EIT. This examination method enabled us to follow the topographical distribution of inspired air in the chest cross-section at the bedside without any disturbance of the spontaneous breathing pattern or change in respiratory mechanics. In spite of the occurrence of periodic breathing, the selection of periods of stable rapid tidal breathing and spontaneous large inspirations, which could be unambiguously identified in all infants, allowed an analysis of regional lung ventilation during well-defined ventilatory states. The study revealed that body position and breathing pattern exert a significant effect on the distribution of lung ventilation during spontaneous breathing in this age group.
Until now, surprisingly little has been known about the topographical distribution of inspired air in the lungs of pre-term and term neonates. In adults, a wealth of data on the spatial inhomogeneity of lung ventilation during both spontaneous and mechanical ventilation exist [15, 16] but only few studies have been carried out in neonates and infants. The lack of adequate techniques and the reluctance to use radioactive tracer gases in otherwise healthy babies is probably one explanation for the limited number of studies performed so far. Besides, the examination techniques applied until now required the use of face masks, intubation and sedation, all of which modify the respiratory mechanics and the breathing pattern, and therefore hardly characterise the true ventilation distribution during undisturbed spontaneous breathing. However, the largest problem of studies on subjects in this age group is the fact that neonates are non-cooperative. In view of these considerations it is no wonder that our knowledge on the spatial distribution of lung ventilation and the effect of body posture on respiration in neonates is limited to data obtained in sedated or anaesthetised infants [17, 18, 19], in infants with lung [17, 19, 20] or other disease [18], during mechanical ventilation [18, 19, 20] and in subject groups with large age heterogeneity [17, 18, 21].
Effect of posture and breathing pattern
It is well known that in adults the dependent lung regions are more ventilated than the non-dependent ones both during quiet tidal breathing and deep inspirations [15]. In the elderly, a reversal of this pattern of distribution of inspired air in lungs occurs due to the loss of lung elastic recoil and collapse of lung regions [15, 22]. A reversal of the adult pattern has also been postulated in infants and it was established in the right and left decubitus positions by gamma camera scanning in a group of mostly ill and mechanically ventilated infants [21]. In our study, no significant differences between the ventilation of the dependent and non-dependent lungs were found in the right lateral posture during rapid tidal breathing, which means that the distribution of inspired air was dissimilar from the adult pattern but it was not reversed. This result is not in conflict with the scintigraphic study mentioned [21]; on the contrary, it provides a new insight into the breathing strategy of neonates.
The mechanics of neonatal breathing differs from the adult one. Due to high chest wall compliance, neonates have significantly lower relative relaxation volumes than adults. Normally, and in contrast with adults, they breathe from end-expiratory lung volumes (VE') that are higher than the relaxation ones. There are several mechanisms like braking of expiration or shortening of expiration time that secure an elevated VE' [13, 14, 23, 24]. It is probable that the infants studied by Davies et al. [21] were sedated during the scintigraphic examinations and the maintenance of normal elevated VE' was suppressed. Under these conditions, the closing of lung units was probable and the pattern of distribution of inspired air in lungs resembled the pattern found in adults breathing at very low volumes below functional residual capacity with preferential ventilation of the non-dependent lung [15]. This distribution pattern may have been further enhanced by applied mechanical ventilation, which is, at least in adults, known to enhance the ventilation of non-dependent lung regions [25]. In our study, mainly due to high respiratory rates with short expiratory times, the ventilation at elevated VE' was present during the selected phases of tidal breathing, resulting in a more homogeneous distribution of ventilation between the dependent and non-dependent lungs.
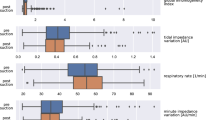
The existence of such ventilatory behaviour is additionally supported by one of our EIT measurements performed in infant 9 (Fig. 6). Initially (~period 1), the neonate breathed at a rate of approximately 48·min–1, and by the end of the scanning period (~period 3) at about 76·min–1. The average end-expiratory-to-end-inspiratory amplitude of relative impedance change, as well as the minimum end-expiratory values, were smaller in period 1 than in period 3, indicating that the infant breathed with lower VT and at a lower VE' in period 1. The functional EIT images of regional ventilation generated from the data obtained in the respective measurement periods showed lower ventilation of the dependent lung region during the low-VT, low-VE' period (period 1), a reduction of the right-to-left imbalance in ventilation at higher VT and higher VE' (period 3) and even a reversal of the ventilation distribution pattern, with the dependent lung being better ventilated during the spontaneous large inspiration (period 2).
EIT measurement in infant 9 in the right lateral posture. The tracing of relative impedance change (left) shows the average data in the chest cross-section. Functional EIT images of regional lung ventilation (right) were generated from the enhanced sections of the measurement and were all scaled to their individual maximum values of end-expiratory-to-end-inspiratory relative impedance change. The fine dotted lines show the average and individual end-expiratory and end-inspiratory data points during tidal breathing or deep inspiration respectively. V T tidal volume, V E' end-expiratory lung volume, fresp breathing rate
Our data showed, for the first time to our knowledge, that the inspired air was preferentially directed towards the dependent lung regions during spontaneous deep breaths in the right lateral posture. Thus, the ventilation distribution under these conditions was identical to the adult pattern. It was interesting to observe that the end-inspiratory area of the dependent lung region increased during such large inspirations (Fig. 5), probably because of an upward movement of the mediastinum. This mechanism has previously been described in adults [25, 26].
The examination of regional lung ventilation in the prone position surprisingly revealed lower ventilation in the left than in the right lung region during tidal breathing. We were not able to find any reference to such a spatial dissimilarity of ventilation or any study on regional lung ventilation in this posture in neonates in the literature, and we can only speculate about the explanation for this finding. In the prone posture, the abdominal wall is compressed, its compliance reduced and, consequently, respiratory mechanics modified [27]. However, this effect alone does not explain the right-to-left difference in ventilation. Our subjects were studied immediately after being fed and we hypothesise that the increased stomach size and/or a change in the heart location elicited a regionally dissimilar effect on local lung mechanics leading to the observed inhomogeneous distribution of air in the lungs. A possible effect of the head position (inconsistent in the present study) on the ventilation distribution can also not be excluded. Because no significant change in the right and left lung areas occurred in this posture (Fig. 5), it is obvious that the reduction of local ventilation was the consequence of locally reduced amplitude of tidal air volume changes. During deep inspirations, this right-to-left difference in regional lung ventilation disappeared.
The analysis of the data acquired during repeated measurements in the supine posture revealed a good reproducibility of the determined spatial distribution of lung ventilation. Thus, the changes in posture performed between the measurements in the initial and last supine position did not affect the pattern of distribution of regional lung ventilation.
Conclusion
Our study provided new information on the neonatal breathing strategy and its effect on regional lung ventilation. Thanks to the use of EIT we could acquire novel data on the spatial distribution of respired air in neonatal lungs. Recently, neonatal breathing has been characterised by Thach [14] as a ventilation with "fast breaths, slow breaths, small breaths, big breaths". On the basis of our data we can add two further characteristics to this definition: "high spatial ventilation inhomogeneity, low spatial ventilation inhomogeneity". Our results show that not only the respiratory rate and VT but also the topography of the distribution of respired air in lungs exhibit high variability in neonates. The distribution of regional ventilation is instantaneously influenced by the breathing pattern and modified by posture.
Our present work showed that EIT examinations of regional lung ventilation are feasible in neonates in the ICU and that they provide information on local lung function not otherwise accessible at the bedside. In contrast with our recent study [9], we have used a modern, technologically advanced EIT device [1], which markedly reduced the electrical noise sensitivity during scanning, enabled higher scan rates and improved the quality of generated EIT images. The present results indicate that future EIT application in critically ill infants may improve the diagnostic and monitoring possibilities in this patient group. A more disease-specific ventilator strategy and optimisation of the weaning procedure have recently been identified as the most important issues in paediatric ventilator therapy [28, 29]. We expect that prospective EIT studies designed to study regional lung ventilation in the course of ventilator therapy and during weaning will improve our understanding of the local effects of mechanical ventilation, establish the ability of EIT to identify regional ventilation inhomogeneities with, for example, atelectasis formation or overdistension, and confirm the usefulness of EIT in neonatal and paediatric intensive care.
References
Hahn G, Thiel F, Dudykevych T, Frerichs I, Gersing E, Schröder T, Hartung C, Hellige G (2001) Quantitative evaluation of the performance of different electrical tomography devices. Biomed Tech 46:91–95
Frerichs I (2000) Electrical impedance tomography (EIT) in applications related to lung and ventilation: a review of experimental and clinical activities. Physiol Meas 21:R1–R21
Frerichs I, Hinz J, Herrmann P, Weisser G, Hahn G, Dudykevych T, Quintel M, Hellige G (2002) Detection of local lung air content by electrical impedance tomography compared with electron beam CT. J Appl Physiol 93:660–666
Hinz J, Neumann P, Hahn G, Maripuu E, Andersson LG, Hellige G, Burchardi H, Hedenstierna G (2000) Electrical impedance tomography measures ventilation distribution: a comparison with ventilation scintigraphy [abstract]. Intensive Care Med 26 [Suppl 3]:292
Hahn G, Šipinková I, Baisch F, Hellige G (1995) Changes in the thoracic impedance distribution under different ventilatory conditions. Physiol Meas 16:A161–A173
Frerichs I, Hahn G, Hellige G (1999) Thoracic electrical impedance tomographic measurements during volume controlled ventilation—effects of tidal volume and positive end-expiratory pressure. IEEE Trans Med Imaging 18:764–773
Kunst PWA, de Vries PMJM, Postmus PE, Bakker J (1999) Evaluation of electrical impedance tomography in the measurement of PEEP–induced changes in lung volume. Chest 115:1102–1106
Frerichs I, Dudykevych T, Hinz J, Bodenstein M, Hahn G, Hellige G (2001) Gravity effects on regional lung ventilation determined by functional EIT during parabolic flights. J Appl Physiol 91:39–50
Frerichs I, Schiffmann H, Hahn G, Hellige G (2001) Non-invasive radiation-free monitoring of regional lung ventilation in critically ill infants. Intensive Care Med 27:1385–1394
Barber DC (1989) A review of image reconstruction techniques for electrical impedance tomography. Med Phys 16:162–169
Kotre CJ (1997) Electrical impedance tomography. Br J Radiol 70:S200–S205
Brown BH (2001) Medical impedance tomography and process impedance tomography: a brief review. Meas Sci Technol 12:991–996
Rigatto H (1992) Control of breathing in fetal life and onset and control of breathing in the neonate. In: Polin RA, Fox WW (eds) Fetal and neonatal physiology. Saunders, Philadelphia, pp 790–800
Thach B (2001) Fast breaths, slow breaths, small breaths, big breaths: importance of vagal innervation in the newborn lung. J Appl Physiol 91:2298–2300
Milic-Emili J (1986) Static distribution of lung volumes. In: Macklem PT, Mead J (eds) Handbook of physiology. Section 3: the respiratory system. Vol III: mechanics of breathing. American Physiological Society, Bethesda, pp 561–574
Rehder K, Marsh HM (1986) Respiratory mechanics during anesthesia and mechanical ventilation. In: Macklem PT, Mead J (eds) Handbook of physiology. Section 3: the respiratory system. Volume III. Mechanics of breathing. American Physiological Society, Bethesda, pp 737–752
Helms P, Hulse MG, Hatch DJ (1982) Lung volume and lung mechanics in infancy lateral or supine posture? Pediatr Res 16:943–947
Larsson A, Jonmarker C, Lindahl SGE, Werner O (1989) Lung function in the supine and lateral decubitus positions in anaesthetized infants and children. Br J Anaesth 62:378–384
Schrod L, Frauendienst-Egger G, von Stockhausen HB (1993) Effect of body position and positioning changes on lung function in premature and newborn infants. Klin Pädiatr 205:145–149
Heaf DP, Helms P, Gordon I, Turner HM (1983) Postural effects on gas exchange in infants. N Engl J Med 308:1505–1508
Davies H, Kitchman R, Gordon I, Helms P (1985) Regional ventilation in infancy. Reversal of adult pattern. N Engl J Med 313:1626–1628
Holland J, Milic-Emili J, Macklem PT, Bates DV (1968) Regional distribution of pulmonary ventilation and perfusion in elderly subjects. J Clin Invest 47:81–92
Kosch PC, Stark AR (1984) Dynamic maintenance of end-expiratory lung volume in full-term infants. J Appl Physiol 57:1126–1133
Stark AR, Cohlan BA, Waggener TB, Frantz ID III, Kosch PC (1987) Regulation of end-expiratory lung volume during sleep in premature infants. J Appl Physiol 62:1117–1123
Froese AB, Bryan AC (1974) Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology 41:242–255
Roussos CS, Martin RR, Engel LA (1977) Diaphragmatic contraction and the gradient of alveolar expansion in the lateral posture. J Appl Physiol 43:32–38
Mortola JP (1992) Measurements of respiratory mechanics. In: Polin RA, Fox WW (eds) Fetal and neonatal physiology. Saunders, Philadelphia, pp 813–821
Rimensberger PC (2002) Neonatal respiratory failure. Curr Opin Pediatr 14:315–321
Brochard L (2001) Weaning from mechanical ventilation. When paediatric intensive care medicine profits from adult experience and vice-versa. Intensive Care Med 27:1564–1566
Acknowledgements
This study was supported by the German Aerospace Centre (DLR) and the German Ministry for Education and Research (BMBF) Grant No. 50 TK 9804.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frerichs, I., Schiffmann, H., Oehler, R. et al. Distribution of lung ventilation in spontaneously breathing neonates lying in different body positions. Intensive Care Med 29, 787–794 (2003). https://doi.org/10.1007/s00134-003-1726-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-003-1726-y