Key Points
-
The serpin superfamily of serine proteinase inhibitors has a central role in controlling proteinases in many biological pathways in a wide range of species. Serpins mediate their effects by a marked conformational transition that inactivates the target proteinase by translocating it from one end of the serpin to the other. This conformational transition is central to the role of serpins as effective antiproteinases but also renders them liable to undergo conformational change that leads to disease (the serpinopathies).
-
The serpinopathies are best characterized by α1-antitrypsin deficiency in humans, which arises from the retention of this serpin in hepatocytes and is associated with liver disease. Biochemical, biophysical, cell-biological and crystallographic studies have shown that α1-antitrypsin deficiency results from the sequential insertion of the reactive-centre loop of one α1-antitrypsin molecule in the β-sheet of another to form chains of polymers. This type of polymerization underlies the deficiency of other mutants of the serpins. For example, antithrombin, C1 inhibitor and α1-antichymotrypsin are associated with thrombosis, angio-oedema and emphysema, respectively.
-
Mutants of the neuron-specific serpin neuroserpin also polymerize by the same mechanism to cause the inclusion body dementia FENIB.
-
There is a striking correlation between the perturbation caused by a mutation, the rate of serpin polymerization and the severity of the clinical phenotype.
-
The polymerization that underlies the serpinopathies — caused by the insertion of the reactive loop into a β-sheet — provides a model for other conformational diseases that result from aberrant β-linkages.
-
The serpinopathies have similarities with the amyloidoses, the prion encephalopathies and Huntington and Alzheimer disease.
Abstract
The serpin superfamily of serine proteinase inhibitors has a central role in controlling proteinases in many biological pathways in a wide range of species. The inhibitory function of the serpins involves a marked conformational transition, but this inherent molecular flexibility also renders the serpins susceptible to point mutations that result in aberrant intermolecular linkage and polymer formation. The effects of such protein aggregation are cumulative, with a progressive loss of cellular function that results in diseases as diverse as cirrhosis and emphysema. The recent recognition that mutations in a serpin can also result in late-onset dementia provides insights into changes that underlie other conformational diseases, such as the amyloidoses, the prion encephalopathies and Huntington and Alzheimer diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Carrell, R. W. & Lomas, D. A. Conformational diseases. Lancet 350, 134–138 (1997).
Kopito, R. R. & Ron, D. Conformational disease. Nature Cell Biol. 2, E207–E209 (2000).
Carrell, R. W. & Lomas, D. A. α1-antitrypsin deficiency: a model for conformational diseases. N. Engl. J. Med. 346, 45–53 (2002).
Tran, P. B. & Miller, R. J. Aggregates in neurodegenerative disease: crowds and power? Trends Neurosci. 22, 194–197 (1999).
Walker, L. C. & LeVine, H. 3rd. The cerebral proteopathies. Neurobiol. Aging 21, 559–561 (2000).
Huntington, J. A., Read, R. J. & Carrell, R. W. Structure of a serpin–protease complex shows inhibition by deformation. Nature 407, 923–926 (2000).The long-sought-after structure of the final complex of a serpin with its target proteinase.
Mast, A. E., Enghild, J. J., Pizzo, S. V. & Salvesen, G. Analysis of the plasma elimination kinetics and conformational stabilities of native, proteinase-complexed, and reactive site cleaved serpins: comparison of α1-proteinase inhibitor, α1-antichymotrypsin, antithrombin III, α2-antiplasmin, angiotensinogen, and ovalbumin. Biochemistry 30, 1723–1730 (1991).
Lomas, D. A., Evans, D. L., Finch, J. T. & Carrell, R. W. The mechanism of Z α1-antitrypsin accumulation in the liver. Nature 357, 605–607 (1992).Shows that the Z variant of α 1 -antitrypsin accumulates in the liver by loop–sheet polymerization.
Stein, P. E. & Carrell, R. W. What do dysfunctional serpins tell us about molecular mobility and disease? Nature Struct. Biol. 2, 96–113 (1995).
Laurell, C.-B. & Eriksson, S. The electrophoretic α1-globulin pattern of serum in α1-antitrypsin deficiency. Scand. J. Clin. Lab. Invest. 15, 132–140 (1963).The first description of plasma deficiency of α 1 -antitrypsin.
Brantly, M., Nukiwa, T. & Crystal, R. G. Molecular basis of α1-antitrypsin deficiency. Am. J. Med. 84 (Suppl. 6A), 13–31 (1988).
Blanco, I., Fernández, E. & Bustillo, E. F. α1-Antitrypsin PI phenotypes S and Z in Europe: an analysis of the published surveys. Clin. Genet. 60, 31–41 (2001).
Sharp, H. L., Bridges, R. A., Krivit, W. & Freier, E. F. Cirrhosis associated with α1-antitrypsin deficiency: a previously unrecognised inherited disorder. J. Lab. Clin. Med. 73, 934–939 (1969).
Sveger, T. The natural history of liver disease in α1-antitrypsin deficient children. Acta Paediatr. Scand. 77, 847–851 (1988).
Eriksson, S., Carlson, J. & Velez, R. Risk of cirrhosis and primary liver cancer in α1-antitrypsin deficiency. N. Engl. J. Med. 314, 736–739 (1986).
Carrell, R. W. et al. Structure and variation of human α1-antitrypsin. Nature 298, 329–334 (1982).
Larsson, C. Natural history and life expectancy in severe α1-antitrypsin deficiency, PiZ. Acta Med. Scand. 204, 345–351 (1978).
Elliott, P. R., Lomas, D. A., Carrell, R. W. & Abrahams, J.-P. Inhibitory conformation of the reactive loop of α1-antitrypsin. Nature Struct. Biol. 3, 676–681 (1996).The crystal structure of α 1 -antitrypsin showed the reactive loop in a conformation that was ideal for docking with the target proteinase. It also provided a model for the structure of α 1 -antitrypsin polymers.
Lomas, D. A., Evans, D. L., Stone, S. R., Chang, W.-S. W. & Carrell, R. W. Effect of the Z mutation on the physical and inhibitory properties of α1-antitrypsin. Biochemistry 32, 500–508 (1993).
Gooptu, B. et al. Inactive conformation of the serpin α1-antichymotrypsin indicates two stage insertion of the reactive loop; implications for inhibitory function and conformational disease. Proc. Natl Acad. Sci. USA 97, 67–72 (2000).
Mahadeva, R., Dafforn, T. R., Carrell, R. W. & Lomas, D. A. Six-mer peptide selectively anneals to a pathogenic serpin conformation and blocks polymerisation: implications for the prevention of Z α1-antitrypsin related cirrhosis. J. Biol. Chem. 277, 6771–6774 (2002).
Sivasothy, P., Dafforn, T. R., Gettins, P. G. W. & Lomas, D. A. Pathogenic α1-antitrypsin polymers are formed by reactive loop–β-sheet A linkage. J. Biol. Chem. 275, 33663–33668 (2000).
Graham, K. S., Le, A. & Sifers, R. N. Accumulation of the insoluble PiZ variant of human α1-antitrypsin within the hepatic endoplasmic reticulum does not elevate the steady-state level of grp78/BiP. J. Biol. Chem. 265, 20463–20468 (1990).
Janciauskiene, S., Dominaitiene, R., Sternby, N. H., Piitulainen, E. & Eriksson, S. Detection of circulating and endothelial cell polymers of Z and wildtype α1-antitrypsin by a monoclonal antibody. J. Biol. Chem. 277, 26540–26546 (2002).
Dafforn, T. R., Mahadeva, R., Elliott, P. R., Sivasothy, P. & Lomas, D. A. A kinetic description of the polymerisation of α1-antitrypsin. J. Biol. Chem. 274, 9548–9555 (1999).
Skinner, R. et al. Implications for function and therapy of a 2.9Å structure of binary-complexed antithrombin. J. Mol. Biol. 283, 9–14 (1998).
Le, A., Ferrell, G. A., Dishon, D. S., Quyen-Quyen, A. L. & Sifers, R. N. Soluble aggregates of the human PiZ α1-antitrypsin variant are degraded within the endoplasmic reticulum by a mechanism sensitive to inhibitors of protein synthesis. J. Biol. Chem. 267, 1072–1080 (1992).
Sidhar, S. K., Lomas, D. A., Carrell, R. W. & Foreman, R. C. Mutations which impede loop/sheet polymerisation enhance the secretion of human α1-antitrypsin deficiency variants. J. Biol. Chem. 270, 8393–8396 (1995).
Wu, Y. et al. A lag in intracellular degradation of mutant α1-antitrypsin correlates with liver disease phenotype in homozygous PiZZ α1-antitrypsin deficiency. Proc. Natl Acad. Sci. USA 91, 9014–9018 (1994).Individuals with Z -α 1 -antitrypsin-related liver disease (as opposed to those with plasma deficiency) have a lag in degrading the retained protein, which indicates that the handling of the polymers is likely to be important in determining which patients develop juvenile cirrhosis.
Cabral, C. M., Liu, Y. & Sifers, R. N. Dissecting the glycoprotein quality control in the secretory pathway. Trends Biochem. Sci. 26, 619–623 (2001).An excellent review that shows the role of glycosylation in determining the fate of α 1 -antitrypsin retained in hepatocytes.
Bruce, D., Perry, D. J., Borg, J.-Y., Carrell, R. W. & Wardell, M. R. Thromboembolic disease due to thermolabile conformational changes of antithrombin Rouen VI (187 Asn→Asp). J. Clin. Invest. 94, 2265–2274 (1994).
Beauchamp, N. J. et al. Antithrombins wibble and wobble (T85M/K): archetypal conformational diseases with in vivo latent-transition, thrombosis and heparin activation. Blood 92, 2696–2706 (1998).
Zhou, A., Huntington, J. A. & Carrell, R. W. Formation of the antithrombin heterodimer and the onset of thrombosis. Blood 94, 3388–3396 (1999).
Corral, J. et al. Molecular characterization of the first homozygous heparin co-factor II deficiency. Involvement in conformational disease. Thrombosis Haemostasis (Suppl.) (2001).
Levashina, E. A. et al. Constitutive activation of toll-mediated antifungal defense in serpin-deficient Drosophila. Science 285, 1917–1919 (1999).
Seyama, K. et al. Siiyama (serine 53 (TCC) to phenylalanine 53 (TTC)). A new α1-antitrypsin-deficient variant with mutation on a predicted conserved residue of the serpin backbone. J. Biol. Chem. 266, 12627–12632 (1991).
Roberts, E. A., Cox, D. W., Medline, A. & Wanless, I. R. Occurrence of α1-antitrypsin deficiency in 155 patients with alcoholic liver disease. Am. J. Clin. Pathol. 82, 424–427 (1984).
Seyama, K., Nukiwa, T., Souma, S., Shimizu, K. & Kira, S. α1-antitrypsin-deficient variant Siiyama (Ser53[TCC] to Phe53[TTC]) is prevalent in Japan. Status of α1-antitrysin deficiency in Japan. Am. Rev. Respir. Dis. 152, 2119–2126 (1995).
Lomas, D. A., Finch, J. T., Seyama, K., Nukiwa, T. & Carrell, R. W. α1-antitrypsin Siiyama (Ser53αPhe); further evidence for intracellular loop–sheet polymerisation. J. Biol. Chem. 268, 15333–15335 (1993).
Lomas, D. A. et al. Alpha1-antitrypsin Mmalton (52Phe deleted) forms loop–sheet polymers in vivo: evidence for the C sheet mechanism of polymerisation. J. Biol. Chem. 270, 16864–16870 (1995).
Millar, D. S. et al. Three novel missense mutations in the antithrombin III (AT3) gene causing recurrent venous thrombosis. Hum. Genet. 94, 509–512 (1994).
Aulak, K. S. et al. A hinge region mutation in C1-inhibitor (Ala436φThr) results in nonsubstrate-like behavior and in polymerization of the molecule. J. Biol. Chem. 268, 18088–18094 (1993).
Eldering, E., Verpy, E., Roem, D., Meo, T. & Tosi, M. COOH-terminal substitutions in the serpin C1 inhibitor that cause loop overinsertion and subsequent multimerization. J. Biol. Chem. 270, 2579–2587 (1995).
Poller, W. et al. A leucine-to-proline substitution causes a defective α1-antichymotrypsin allele associated with familial obstructive lung disease. Genomics 17, 740–743 (1993).
Elliott, P. R., Stein, P. E., Bilton, D., Carrell, R. W. & Lomas, D. A. Structural explanation for the dysfunction of S α1-antitrypsin. Nature Struct. Biol. 3, 910–911 (1996).
Mahadeva, R. et al. Heteropolymerisation of S, I and Z α1-antitrypsin and liver cirrhosis. J. Clin. Invest. 103, 999–1006 (1999).
Davis, R. L. et al. Familial encephalopathy with neuroserpin inclusion bodies (FEN1B). Am. J. Pathol. 155, 1901–1913 (1999).
Davis, R. L. et al. Familial dementia caused by polymerisation of mutant neuroserpin. Nature 401, 376–379 (1999).Demonstration that polymerization of two mutants of neuroserpin underlie a novel inclusion body dementia. The protein linkage is the same as that which underlies the retention of Z α 1 -antitrypsin in hepatocytes to cause cirrhosis.
Bradshaw, C. B. et al. Cognitive deficits associated with a recently reported familial neurodegenerative disease. Arch. Neurol. 58, 1429–1434 (2001).
Belorgey, D., Crowther, D. C., Mahadeva, R. & Lomas, D. A. Mutant neuroserpin (S49P) that causes familial encephalopathy with neuroserpin inclusion bodies is a poor proteinase inhibitor and readily forms polymers in vitro. J. Biol. Chem. 277, 17367–17373 (2002).
Davis, R. L. et al. Association between conformational mutations in neuroserpin and onset and severity of dementia. Lancet 359, 2242–2247 (2002).
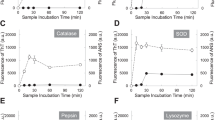
Abrahamson, M. & Grubb, A. Increased body temperature accelerates aggregation of the Leu–68φGln mutant cystatin C, the amyloid-forming protein in hereditary cystatin C amyloid angiopathy. Proc. Natl Acad. Sci. USA 91, 1416–1420 (1994).
Janowski, R. et al. Human cystatin C, an amyloidogenic protein dimerizes through three-dimensional domain swapping. Nature Struct. Biol. 8, 316–320 (2001).
Staniforth, R. A. et al. Three-dimensional domain swapping in the folded and molten-globule states of cystatins, an amyloid-forming structural superfamily. EMBO J. 20, 4774–4781 (2001).
McParland, V. J., Kalverda, A. P., Homans, S. W. & Radford, S. E. Structural properties of an amyloid precursor of β2-microglobulin. Nature Struct. Biol. 9, 326–331 (2002).
Booth, D. R. et al. Instability, unfolding and aggregation of human lysozyme variants underlying amyloid fibrillogenesis. Nature 385, 787–793 (1997).
Lashuel, H. A., Wurth, C., Woo, L. & Kelly, J. W. The most pathogenic transthyretin variant, L55P, forms amyloid fibrils under acidic conditions and protofilaments under physiological conditions. Biochemistry 12, 13560–13573 (1999).
Eanes, E. D. & Glenner, G. G. X-ray diffraction studies on amyloid filaments. J. Histochem. Cytochem. 16, 673–677 (1968).
Blake, C. & Serpell, L. Synchrotron X-ray studies suggest that the core of the transthyretin amyloid fibril is a continuous β-sheet helix. Structure 4, 989–998 (1996).Interpretation of the diffraction pattern of amyloid fibrils, with a satisfying model for their structure.
Sunde, M. et al. Common core structure of amyloid fibrils by synchrotron X-ray diffraction. J. Mol. Biol. 273, 729–739 (1997).
Pepys, M. B. Pathogenesis, diagnosis and treatment of systemic amyloidosis. Phil. Trans. R. Soc. Lond. B Biol. Sci. 356, 203–210 (2001).
Walsh, D. M., Lomakin, A., Benedek, G. B., Condron, M. M. & Teplow, D. B. Amyloid β-protein fibrillogenesis. Detection of a protofibrillar intermediate. J. Biol. Chem. 272, 22364–22372 (1997).
Goldberg, M. S. & Lansbury, P. T. J. Is there a cause-and-effect relationship between α-synuclein fibrillization and Parkinson's disease? Nature Cell Biol. 2, E115–E119 (2000).
Fraser, P. E. et al. Fibril formation by primate, rodent, and Dutch-hemorrhagic analogues of Alzheimer amyloid β-protein. Biochemistry 31, 10716–10723 (1992).
Iversen, L. L., Mortishire-Smith, R. J., Pollack, S. J. & Shearman, M. S. The toxicity in vitro of β-amyloid protein. Biochem. J. 311, 1–16 (1995).
Polymeropoulos, M. H. et al. Mutations in the α-synuclein gene identified in families with Parkinson's disease. Science 276, 2045–2047 (1997).
Kruger, R. et al. Ala30Pro mutation in the gene encoding α-synuclein in Parkinson's disease. Nature Genet. 18, 106–108 (1998).
Spillantini, M. G., Crowther, R. A., Jakes, R., Hasegawa, M. & Goedert, M. α-Synuclein in filamentous inclusions of Lewy bodies from Parkinson's disease and dementia with lewy bodies. Proc. Natl Acad. Sci. USA 95, 6469–6473 (1998).
Conway, K. A. et al. Acceleration of oligomerization, not fibrillization, is a shared property of both α-synuclein mutations linked to early-onset Parkinson's disease: implications for pathogenesis and therapy. Proc. Natl Acad. Sci. USA 97, 571–576 (2000).
Knaus, K. J. et al. Crystal structure of the human prion protein reveals a mechanism of oligomerization. Nature Struct. Biol. 8, 770–774 (2001).
Emmerich, J. et al. A phenylalanine 402 to leucine mutation is responsible for a stable inactive conformation of antithrombin. Thromb. Res. 76, 307–315 (1994).
Kelly, J. W. Mechanisms of amyloidogenesis. Nature Struct. Biol. 7, 824–826 (2000).
Bousset, L., Thomson, N. H., Radford, S. E. & Melki, R. The yeast prion Ure2p retains its native alpha-helical conformation upon assembly into protein fibrils in vitro. EMBO J. 21, 2903–2911 (2002).
Huntington, J. A. et al. A 2.6Å structure of a serpin polymer and implications for conformational disease. J. Mol. Biol. 293, 449–455 (1999).
Dunstone, M. A. et al. Cleaved antitrypsin polymers at atomic resolution. Protein Sci. 9, 417–420 (2000).
Iwata, N. et al. Metabolic regulation of brain Aβ by neprilysin. Science 292, 1550–1552 (2001).
Kitada, T. et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature 392, 605–608 (1998).
Haass, C., Hung, A. Y., Schlossmacher, M. G., Teplow, D. B. & Selkoe, D. J. β-Amyloid peptide and a 3-kDa fragment are derived by distinct cellular mechanisms. J. Biol. Chem. 268, 3021–3024 (1993).
Haass, C. et al. Amyloid β-peptide is produced by cultured cells during normal metabolism. Nature 359, 322–325 (1992).
Shoji, M. et al. Production of the Alzheimer amyloid β protein by normal proteolytic processing. Science 258, 126–129 (1992).
Selkoe, D. J. Alzheimer's disease: genes, proteins and therapy. Physiol. Rev. 81, 741–766 (2001).
Wolfe, M. S. et al. Two transmembrane aspartates in presenilin-1 required for presenilin endoproteolysis and β-secretase activity. Nature 398, 513–517 (1999).
Li, Y.-M. et al. Photoactivated α-secretase inhibitors directed to the active site covalently label presenilin 1. Nature 405, 689–694 (2000).
Sinha, S. et al. Purification and cloning of amyloid precursor protein β-secretase from human brain. Nature 402, 537–540 (1999).
Yan, R. et al. Membrane-anchored aspartyl protease with Alzheimer's disease β-secretase activity. Nature 402, 533–537 (1999).
Vassar, R. et al. Beta-secretase cleavage of Alzheimer's amyloid precursor protein by the transmembrane aspartic protease BACE. Science 286, 735–741 (1999).
Hussain, I. et al. Identification of a novel aspartic protease (Asp 2) as β-secretase. Mol. Cell. Neurosci. 14, 419–427 (1999).
Muchowski, P. J. et al. Hsp70 and Hsp40 chaperones can inhibit self-assembly of polyglutamine proteins into amyloid-like fibrils. Proc. Natl Acad. Sci. USA 97, 7841–7846 (2002).
Perutz, M. F. Glutamine repeats and inherited neurodegenerative diseases: molecular aspects. Curr. Opin. Struct. Biol. 6, 848–858 (1996).
Perutz, M. F., Finch, J. T., Berriman, J. & Lesk, A. Amyloid fibres are water-filled nanotubes. Proc. Natl Acad. Sci USA 99, 5591–5595 (2002).
Soto, C. et al. β-Sheet breaker peptides inhibit fibrillogenesis in a rat brain model of amyloidosis: implications for Alzheimer's therapy. Nature Med. 4, 822–826 (1998).Demonstration that small peptides can block the β-strand linkage of the peptide that is thought to cause Alzheimer disease and so reduce plaque formation in an animal model.
Devlin, G. L., Parfrey, H., Tew, D. J., Lomas, D. A. & Bottomley, S. P. Prevention of polymerization of M and Z α1-antitrypsin (α1-AT) with trimethylamine N-oxide. Implications for the treatment of α1-AT deficiency. Am. J. Respir. Cell Mol. Biol. 24, 727–732 (2001).
Pepys, M. B. et al. Targeted pharmacological depletion of serum amyloid P component for treatment of human amyloidosis. Nature 417, 254–259 (2002).Elegant demonstration of the use of rational drug design to develop a drug for the treatment of the amyloidoses.
Bard, F. et al. Peripherally administered antibodies against amyloid β-peptide enter the central nervous system and reduce pathology in a mouse model of Alzheimer disease. Nature Med. 6, 916–919 (2000).
Burrows, J. A. J., Willis, L. K. & Perlmutter, D. H. Chemical chaperones mediate increased secretion of mutant α1-antitrypsin (α1-AT) Z: a potential pharmacologcial strategy for prevention of liver injury and emphysema. Proc. Natl Acad. Sci. USA 97, 1796–1801 (2000).
Morgan, D. et al. Aβ peptide vaccination prevents memory loss in an animal model of Alzheimer's disease. Nature 408, 982–985 (2000).
Fitton, H. L., Pike, R. N., Carrell, R. W. & Chang, W.-S. W. Mechanisms of antithrombin polymerisation and heparin activation probed by insertion of synthetic reactive loop peptides. Biol. Chem. 378, 1059–1063 (1997).
Chang, W.-S. W., Wardell, M. R., Lomas, D. A. & Carrell, R. W. Probing serpin reactive loop conformations by proteolytic cleavage. Biochem. J. 314, 647–653 (1996).
Elliott, P. R., Pei, X. Y., Dafforn, T. R. & Lomas, D. A. Topography of a 2.0Å structure of α1-antitrypsin reveals targets for rational drug design to prevent conformational disease. Protein Sci. 9, 1274–1281 (2000).
Rubenstein, R. C. & Zeitlin, P. L. A pilot clinical trial of oral sodium 4-phenylbutyrate (Buphenyl) in ΔF508-homozygous cystic fibrosis patients: partial restoration of nasal epithelial CFTR function. Am. J. Respir. Crit. Care Med. 157, 484–490 (1998).
Author information
Authors and Affiliations
Corresponding author
Related links
Related links
DATABASES
LocusLink
cystic fibrosis transmembrane regulator
plasminogen activator inhibitor 1
OMIM
familial encephalopathy with neuroserpin inclusion bodies
FURTHER INFORMATION
Glossary
- β-LINKAGE
-
Intermolecular bonding between β-strands. In some cases, this might result from aligned β-strands, but in others, it arises from domain swaps; that is, the incorporation of a β-strand from one molecule into a β-sheet of another.
- β-SHEETS
-
A polypeptide chain can fold back and forth on itself, with the strands being held together by interlinking hydrogen bonds with the peptide groups of neighbouring strands. This provides a very rigid structure that forms the core of many (but not all) proteins.
- COMPLEMENT CASCADE
-
A proteolytic cascade that protects the host against infection. The components of the complement pathway coat and kill invading organisms and release inflammatory mediators. Its activation is controlled by the serpin C1 inhibitor.
- FIBRINOLYTIC CASCADE
-
The breakdown (or lysis) of fibrin, which is the final product of the clotting cascade.
- PSEUDOSUBSTRATE
-
A peptide sequence that is recognized by the enzyme as a substrate, but which then inactivates the proteinase.
- ISOELECTRIC FOCUSING GELS
-
Thin-layer acrylamide gels that separate proteins by mass and charge. The different mutants of α1-antitrypsin have characteristic migration profiles.
- PERIODIC ACID SCHIFF REACTION
-
(PAS). Periodic acid oxidizes some polysaccharides to produce aldehydes that react with the Schiff reagent. Inclusions of mutants of α1-antitrypsin in hepatocytes and mutants of neuroserpin in neurons stain positive for PAS but are resistant to treatment with salivary amylase (diastase).
- CIRRHOSIS
-
Diffuse damage and fibrosis of the liver that is associated with nodules of regenerating hepatocytes. The common causes include chronic infection with hepatitis viruses B and C and prolonged alcohol abuse. It might also result from the accumulation of the Z variant of α1-antitrypsin.
- SHUTTER DOMAIN
-
The region of a serpin that controls opening of the A-sheet and acceptance of the reactive centre loop. Mutations in this domain allow the acceptance of the reactive loop of another molecule and hence the formation of polymers.
- ANGIO-OEDEMA
-
A clinical syndrome that results from a true or functional deficiency of the plasma protein C1 inhibitor. The deficiency results in unchecked activation of the complement cascade and the production of vasoactive mediators. It might have an autosomal-dominant pattern of inheritance and is characterized by swelling of the skin, bowel and larynx.
- EMPHYSEMA
-
Abnormal enlargement of the airspaces (alveoli) after they divide from the terminal bronchi (airways). The most common cause is smoking but genetic deficiency of α1-antitrypsin predisposes some individuals to emphysema at an early age.
- EOSINOPHILIC
-
Containing the white blood cells eosinophils. The cytoplasm of eosinophils is filled with coarse, refractile granules that stain intensely with acid dyes.
- SUBSTANTIA NIGRA
-
A pigmented band of grey matter in the midbrain. Neuronal degeneration of this tract results in Parkinson disease, which is characterized by a slow tremor, rigidity and difficulty in initiating movements.
- BIREFRINGENCE
-
The splitting of an incident wave into two waves of different velocities and orthogonal polarizations.
- DOPAMINE
-
A chemical neurotransmitter that is found in high concentrations in the substantia nigra.
- CHAPERONES
-
A protein that aids the folding of another to prevent it from taking an inactive conformation.
Rights and permissions
About this article
Cite this article
Lomas, D., Carrell, R. Serpinopathies and the conformational dementias. Nat Rev Genet 3, 759–768 (2002). https://doi.org/10.1038/nrg907
Issue Date:
DOI: https://doi.org/10.1038/nrg907
This article is cited by
-
Cerebrospinal fluid shotgun proteomics identifies distinct proteomic patterns in cerebral amyloid angiopathy rodent models and human patients
Acta Neuropathologica Communications (2024)
-
Polymerogenic neuroserpin causes mitochondrial alterations and activates NFκB but not the UPR in a neuronal model of neurodegeneration FENIB
Cellular and Molecular Life Sciences (2022)
-
G392E neuroserpin causing the dementia FENIB is secreted from cells but is not synaptotoxic
Scientific Reports (2021)
-
Smoothing a rugged protein folding landscape by sequence-based redesign
Scientific Reports (2016)
-
Embelin binds to human neuroserpin and impairs its polymerisation
Scientific Reports (2016)