Abstract
Objective
To compare the length of hospital stay (primary) and improvement in clinical severity scores (secondary) among children with bronchiolitis nebulized with 3 % hypertonic saline or 0.9% saline.
Design
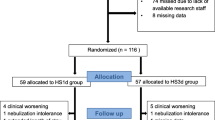
Randomized double blind controlled trial.
Setting
Tertiary care teaching hospital.
Patients
Hospitalized children (1–24 months) with acute bronchiolitis of moderate severity.
Intervention
Nebulization of 4 ml of 3% hypertonic saline or 4 mL of 0.9% saline, along with 2.5 mg salbutamol, at 4-hourly intervals till the patient was ready for discharge.
Results
Baseline characteristics were similar in two groups. Median clinical severity score at admission was 6 (IQR-1) in both the groups. Clinical severity scores monitored afterwards 12-hourly till discharge (132 h) did not show statistically significant differences in 3% and 0.9% saline groups. Mean length of hospital stay (time to reach predefined clinical severity score<3) was 63.93 ± 22.43 h in 3% saline group and 63.51 ± 21.27 h in 0.9% saline group (P=0.878). No adverse events were reported by the parents, caregivers or treating medical attendants in both groups.
Conclusion
Nebulized 3 % saline is not superior to 0.9% saline in infants with clinically diagnosed acute bronchiolitis.
Similar content being viewed by others
References
Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics. 2008; 121:244–252.
Deshpande S, Northern V. The clinical and health economic burden of respiratory syncytial virus disease among children under 2 years of age in a defined geographical area. Arch Dis Child. 2003; 88: 1065–1069.
Zorc JJ, Breese HC. Bronchiolitis: Recent evidence on diagnosis and management. Pediatrics. 2010; 125; 342–349.
Subcommittee on Diagnosis and Management of Bronchiolitis. Clinical Practice Guideline: Diagnosis and Management of Bronchiolitis, American Academy of Pediatrics. Pediatrics. 2006; 118:1774–1793.
Gadomski AM, Bhasale AL. Bronchodilators for bronchiolitis. Cochrane Database Syst Rev. 2006, 3: CD001266.
Hartling L, Bialy LM, Vandermeer B, Tjosvold L, Johnson DW, Plint AC, et al. Epinephrine for bronchiolitis. Cochrane Database Syst Rev. 2011;6:CD003123.
Patel H, Platt R, Lozano JM, Wang EE. Glucocorticoids for acute viral bronchiolitis in infants in infants and young children. Cochrane Database Syst Rev. 2004;3:CD004878.
Perrotta C, Ortiz Z, Roque M. Chest physiotherapy for acute bronchiolitis in pediatric patients between 0 and 24 months old. Cochrane Database Syst Rev 2006; 1: 004873.
Landrigan CP, Conway PH, Stucky ER, Chiang VW, Ottolini MC. Variation in pediatric hospitalists’ use of proven and unproven therapies: a study from the Pediatric Research in Inpatient Settings (PRIS) Network. J Hosp Med. 2008; 3:292–298.
Mandelberg A, Tal G, Witzling M, Someck E, Houri S, Balin A, et al. Nebulized 3% hypertonic saline solution treatment in hospitalized infants with viral bronchiolitis. Chest. 2003; 123: 481–487.
Grewal S, Ali S, McConnell DW, Vandermeer B, Klassen TP. A randomized trial of nebulized 3% hypertonic saline with epinephrine in the treatment of acute bronchiolitis in the emergency department. Arch Pediatr Adolesc Med. 2009;163:1007–1012.
Anil AB, Anil M, Saglam AB, Cetin N, Bal A, Aksu N. High volume normal saline alone is as effective as nebulized salbutamol-normal saline, epinephrine-normal saline, and 3% saline in mild bronchiolitis. Pediatric Pulmonol. 2010;45:41–47.
Zhang L, Mendoza-Sassi RA, Wainwright C, Klassen TP. Nebulized hypertonic saline solution for acute bronchiolitis in infants. Cochrane Database Syst Rev. 2008;4:CD006458.
Sarrell EM, Tal G, Witzling M, Someck E, Houri S, Cohen HA, et al. Nebulized 3% hypertonic saline solution treatment in ambulatory children with viral bronchiolitis decreases symptoms. Chest. 2002; 122: 2015–2020.
Tal G, Cesar K, Houri S, Ballin A, Mandelberg A. Hypertonic saline/epinephrine treatment in hospitalized infants with viral bronchiolitis reduces hospitalizations stay: 2 years experience. Isr Med Assoc J. 2006; 8:169–173.
Kuzik BA, Al Qaghi SA, Kent S, Flavin MP, Hopman W, Hotte S, et al. Nebulized hypertonic saline in the treatment of viral bronchiolitis in infants. J Pediatr. 2007; 151: 266–270.
Luo Z, Liu E, Luo J, Li S, Zeng F, Yang X, et al. Nebulized hypertonic saline/salbutamol solution treatment in hospitalized children with mild to moderate bronchiolitis. Pediatr Int. 2010;52:199–202.
Khalid AA, Sakran M, Bruce L, Davidson, Sayyed RE, Mahjoub H, et al. Nebulized 5% or 3% hypertonic or 0.9% saline for treating acute bronchiolitis in infants. J Pediatr. 2010;157:630–634.
Luo Z, Fu Z, Liu E, Xu X, Fu X, Peng D, et al. A randomized controlled trial of nebulized hypertonic saline treatment in hospitalized children with moderate to severe viral bronchiolitis. Clin Microbiol Infect. Clin Microbiol Infect. 2011;17:1829–1833.
Daviskas E, Anderson SD, Gonda I, Eberl S, Meikle S, Seale JP, et al. Inhalation of hypertonic saline aerosol enhances mucociliary clearance in asthmatic and healthy subjects. European Resp J. 1996;9:725–732.
Wark P, McDonald V, Jones A. Nebulised hypertonic saline for cystic fibrosis. Cochrane Database Syst Rev. 2007;4:CD001506.
Tarran R, Donaldson S, Boucher RS. Rationale for hypertonic saline therapy for cystic fibrosis lung disease. Semin Respir Crit Care Med. 2007;28: 295–302.
Kellett 2005 Kellett F, Redfern J, Niven RM. Evaluation of nebulised hypertonic saline (7%) as an adjunct to physiotherapy in patients with stable bronchiectasis. Resp Med. 2005;991:27–31.
Shoseyov D, Bibi H, Shai P, Ahoseyov N, Shazberg G, Hurvitz H. Treatment with hypertonic saline versus normal saline nasal wash of pediatric chronic sinusitis. J.Allergy and Clin Immunol. 1998;101:602–605.
Wang EE, Milner RA, Navas L, Maj H. Observer agreement for respiratory signs and oximetry in infants hospitalized with lower respiratory infections. Am Rev Resp Dis. 1992;145:106–109.
Ralston S, Hill V, Martinez M. Nebulized hypertonic saline without adjunctive bronchodilators for children with bronchiolitis. Pediatrics. 2010;126:e520–525.
Horner D, Bartram T, Jenner R Morton R. Can the efficacy of hypertonic saline in bronchiolitis truly be assessed with a short-term primary outcome? Arch Pediatr Adolesc Med. 2010; 164:395.
Sood N, Bennett WD, Zeman K, Brown J, Foy C, Boucher RC, et al. Increasing concentration of inhaled saline with or without amiloride: effect on: mucociliary clearance in normal subjects. Am J Respir Crit Care Med. 2003;167:158–163.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharma, B.S., Gupta, M.K. & Rafik, S.P. Hypertonic (3%) saline Vs 0.9% saline nebulization for acute viral bronchiolitis: A randomized controlled trial . Indian Pediatr 50, 743–747 (2013). https://doi.org/10.1007/s13312-013-0216-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-013-0216-8