Abstract
Purpose
To assess whether obesity is associated with mortality or other adverse intensive care unit (ICU) and post-ICU outcomes.
Methods
A meta-analysis of studies from PubMed and EMBASE databases.
Results
Twenty-two studies (n = 88,051 patients) were included. Pooled analysis demonstrated no difference in ICU mortality, but lower hospital mortality for obese and morbidly obese subjects (RR 0.76; 95% CI 0.59, 0.92; RR 0.83; 95% CI 0.66, 1.04, respectively) versus normal weight subjects. There was no association between obesity and duration of mechanical ventilation or ICU stay. Morbidly obese versus normal weight patients had longer hospitalizations. No study reported physical function, mental health, or quality of life outcomes after discharge.
Conclusions
Obesity is not associated with increased risk for ICU mortality, but may be associated with lower hospital mortality. There is a critical lack of research on how obesity may affect complications of critical illness and patient long-term outcomes.
Similar content being viewed by others
Introduction
Nearly one-third of intensive care unit (ICU) patients are obese and nearly 7% are morbidly obese, frequencies that are predicted to increase as the prevalence of obesity in the general population rises [1, 2]. Thus, understanding the consequences of obesity on critical illness has great public health importance. In the general population, obesity is associated with increased risk for mortality and excess costs of care [3, 4]. Although frequently studied as a chronic disease, the influence of obesity on acute illnesses is poorly understood. Given the rising prevalence of obese patients in ICUs, this issue is especially important in critical care.
Obesity is associated with multiple co-morbid conditions and physiologic derangements (e.g., pro-inflammatory state, insulin resistance), physical limitations, and pharmacokinetic alterations that may complicate acute illness and impede the implementation and/or efficacy of evidence-based interventions in the ICU [5, 6]. Nonetheless, little is known regarding the impact of obesity on short- and long-term outcomes from critical illness. We identified two systematic reviews that examined the role of obesity on ICU and hospital mortality [1, 2]. Akinnusi et al. [1] reported that obesity [body mass index (BMI) ≥30 kg/m2 of body surface area] was not associated with crude ICU mortality. Of note, in that meta-analysis, the reference group for comparisons was non-obese (BMI <30 kg/m2) patients rather than normal weight patients. Prior studies suggest that the relationship between BMI and patient outcomes is “U” shaped [7–13] with worse outcomes for both underweight (BMI <18.5 kg/m2) and morbidly obese (>40 kg/m2) patients. Hence, inclusion of underweight patients in the reference group and morbidly obese patients in the obese group might conceivably bias the results. In their meta-analysis, Oliveros et al. [2] used a reference group of normal weight patients (BMI 18.5–24.9 kg/m2), however, they combined data for ICU and hospital mortality. These investigators found a lower mortality for obese (BMI 30.0–39.9 kg/m2), but not morbidly obese (BMI ≥40 kg/m2) patients. There were inconclusive results from both studies on whether obesity or morbid obesity is associated with prolonged mechanical ventilation or extended ICU length of stay compared with non-obese or normal weight patients. Importantly, although the importance and study of long-term outcomes after critical illness has grown, whether obesity impacts these outcomes were not examined in these prior analysis [14–16].
Our objective was to perform a systematic review of the literature and meta-analysis to evaluate whether obesity impacts the risk for ICU or hospital mortality as well as long-term patient outcomes including physical function and quality of life compared with normal weight patients. We further sought to assess whether obesity affects the duration of mechanical ventilation, ICU and hospital length of stay, and ICU complications.
Methods
Data sources and searches
Relevant English-language publications were identified by searching PubMed and EMBASE databases (as of 10 March 2008) using text words and controlled vocabulary terms, including intensive care, critical care, critical illness, obesity and body weight. No limit by date was used in the search strategy. References from identified citations and relevant review articles were hand searched for additional eligible citations.
Study selection
Criteria for inclusion of publications in this systematic review were: (1) a quantitative comparison of outcomes between obese and non-obese subjects, (2) adult subjects (i.e., <16 years of age), and (3) subjects admitted to an ICU. Publications were excluded if: (1) there were no original data (e.g., review, commentary), (2) a full-length publication was not reported (e.g., abstract only) in a peer-reviewed journal, (3) obese adult ICU patients were not the primary focus, or (4) there were no data on mortality.
Based on these criteria, each title and/or abstract retrieved from the electronic database search was screened for eligibility independently by two of four reviewers (CH, JS, TS, NM). The full text of potentially eligible papers were independently reviewed by two investigators (CH, JS). For eligible publications, relevant data were abstracted. Data abstraction for methodological aspects of studies include: study design, sample size, and study quality (described later). Data on exposures and potential confounders included: definitions of weight categories evaluated (in kg/m2), and severity of illness and organ dysfunction scoring. When available, data was collected on the following outcomes (including outcomes after hospital discharge when applicable): mortality rate in the ICU and hospital; duration of mechanical ventilation, ICU and hospital length of stay; presence of deep venous thrombosis, pulmonary embolism, systemic inflammatory response syndrome (SIRS), catheter-related blood stream infections, sepsis, and acute respiratory distress syndrome; acute renal failure; multiple organ failure; destination after hospital discharge; physical function and quality of life. The methodological quality of eligible studies was assessed using a modified Newcastle–Ottawa scale, a validated instrument designed to evaluate the quality of observational studies in systematic reviews and meta-analyses [17, 18]. Using this scale, methodology was evaluated in three domains: the selection of study groups, the comparability of groups, and the quality of ascertainment of either the exposures (for case–control studies) or of the outcomes (for cohort studies). In the event of unclear or missing data, attempts were made to contact the authors of the publication. Replies were received from the authors of four reports [8, 19–21].
Data synthesis
Because outcomes may vary for under-weight versus normal weight subjects, quantitative synthesis (i.e., meta-analysis) of the data was limited to those studies using a reference group of normal weight subjects, specifically excluding underweight patients (<18.5 kg/m2). A Bayesian model was used to pool data across studies within weight categories while allowing for study to study differences in the outcome measures. Specifically, for ICU and hospital mortality, we extracted the total number of subjects and the number of deaths in each study and each weight category. For each study, this data was incorporated into a binomial regression model with a log link in order to model the log relative risk of mortality across the weight categories (normal weight as the reference group). These estimates of the log relative risk with the corresponding variance estimates represent the maximum likelihood estimates (MLEs) of the study specific associations between mortality and the weight categories. These MLEs were then incorporated into a two-stage normal–normal model in which we estimated a pooled log relative risk for each weight category (normal weight as the reference group) with corresponding 95% credible intervals (CI). We define a significant result to be a 95% CI that does not include a relative risk of 1. To evaluate statistical heterogeneity, we utilized the I 2 statistic which represents the proportion of total variation in the log relative risks that is attributable to heterogeneity across studies [22]. An I 2 of 0 indicates no heterogeneity in the true log relative risks across studies with all variation attributable to within-study statistical uncertainty. An I 2 close to 1 indicates large heterogeneity across studies which indicate large differences across the studies which may be due to mortality differences or inherent differences in the study populations, study designs, patient severity, etc. For duration of mechanical ventilation, and ICU and hospital stay, we extracted the mean and standard deviation duration for each study and each weight category. For studies that reported the durations of mechanical ventilation and ICU and hospital stay with only a range, rather than a standard deviation, we estimated the standard deviation by taking the largest difference between the mean and minimum/maximum and dividing by two. To address the potential effect of estimating the standard deviation, we performed a sensitivity analysis of the results excluding those studies which did not report the standard deviation. Thereafter the analysis of these non-mortality outcomes was completed in a similar fashion to analysis of mortality data. We define a significant result to be a 95% credible interval for the difference in mean duration that does not include zero. Statistical analyses were conducted using R (version 2.7.0) and WinBugs (version 1.4.3) software.
Results
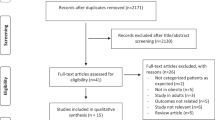
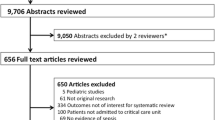
The initial literature search retrieved 1,524 citations. Review of titles, abstracts, and full-length articles resulted in selection of 23 eligible publications (Fig. 1). The studies included 14 retrospective cohort, 6 prospective cohort, and 3 case control studies and they included a wide variety of critically ill patients and sample sizes (Table 1) [7–13, 19–21, 23–35]. The studies by Marik et al. [7] and Tremblay et al. [20] both obtained data from the Project IMPACT database and included significant overlap in the patients populations; hence, only the former study was included in the quantitative synthesis since it encompassed a larger sample size and reported more outcomes. Consequently, this review included data from 88,051 patients with the studies by Marik et al. [7] and Finkielman et al. [8] contributing 48,176 and 19,669 patients (77% of the total sample), respectively. Our assessment of the methodological quality of the cohort studies is provided in Table 2 and for case-control studies in Table 3. Only three of the cohort studies reported masking of the outcome assessor [7, 23, 34] and only four studies were assessed as having a representative cohort [13, 21, 34, 35]. Of the three case-control studies, only one provided an adequate case definition [32].Thirteen studies included multiple BMI categories compared to a reference group of normal weight (excluding underweight) patients, seven studies compared obese versus non-obese (including underweight) patients, and three studies compared normal weight versus overweight patients with only a single category of obesity (≥30 kg/m2).
Mortality
Mortality and other hospital outcomes for the eligible studies are summarized in Table 4. Six studies reported a positive association between obesity or morbid obesity and ICU and/or hospital mortality after risk adjustment [11, 25, 26, 31–33]. In ten studies, obesity was not related [7, 19, 20, 23, 24, 28–31, 34] or in four studies it was protective from risk-adjusted mortality [8, 9, 12, 35]. Two studies did not report risk adjusted mortality outcomes [8–10, 12, 13, 27, 35]. Compared to other BMI categories, underweight patients (<18.5 kg/m2) had higher hospital mortality in four studies [7–9, 13].
We pooled data from eight and nine studies that provided ICU and hospital mortality results, respectively, by BMI categories (Fig. 2). With ICU mortality, we found no significant difference comparing underweight, overweight, obese, and morbidly obese subjects to the normal weight subjects. With hospital mortality, obese patients had lower mortality versus normal weight patients (RR 0.76; 95% credible interval, 0.59, 0.92). Although not statistically significant, similar trends toward decreased hospital mortality also were observed in the pooled estimates for overweight (RR 0.89, 95% credible interval, 0.74, 1.07) and morbidly obese (RR 0.83; 95% CI, 0.66, 1.04) subjects, while underweight subjects had a trend toward increased hospital mortality (RR 1.11; 95% CI, 0.86, 1.39) versus the normal weight reference group. The I 2 statistic for heterogeneity ranged from 50% (morbidly obese vs. normal) to 80% (underweight vs. normal) for ICU mortality and from 86% (underweight vs. normal) to 93% (obese vs. normal) for hospital mortality indicating the need for caution in interpreting pooled estimates due to important differences across the studies.
Forest plots showing the relative risk of ICU and hospital mortality comparing underweight, overweight, obese, and morbidly obese patients to the normal weight patients. For each comparison, we display the Bayesian pooled estimate of relative risk with 95% credible intervals calculated using maximum likelihood estimation
Duration of mechanical ventilation
The rate of mechanical lung ventilation in obese versus non-obese patients was reported in seven studies [10, 26, 27, 31, 33–35]. In a non-risk adjusted analysis, obesity was associated with a higher rate of mechanical ventilation in two studies [27, 31] while no relationship between BMI and rates of mechanical ventilation was found in the remaining studies. No study reported a risk-adjusted analysis of duration of mechanical ventilation by weight category. Five studies reported a longer duration of mechanical ventilation for obese versus normal weight patients [24, 26, 29, 31, 35] while three other studies reported no difference (Table 4) [12, 33, 34]. In our pooled analysis, we found no difference in the duration of mechanical ventilation comparing each weight category to normal weight patients (Fig. 3). The sensitivity analysis of our results (i.e., removing those studies without estimates of standard deviation) did not change these findings. The I 2 statistic for heterogeneity in the mean differences comparing the overweight and obese subjects to normal weight subjects is 74 and 58%, respectively, indicating the need for caution in interpreting these pooled estimates. However, for the underweight and morbidly obese comparisons the I 2 statistic was 10% indicating a low level of statistical heterogeneity across studies.
Forest plots showing the estimated difference in mean days of mechanical ventilation comparing underweight, overweight, obese and morbidly obese patients to normal weight patients. For each comparison, we display the Bayesian pooled estimate of difference in mean days with 95% credible intervals calculated using maximum likelihood estimates
Length of hospitalization
No study reported a risk-adjusted analysis of hospital length of stay by weight category. Twelve studies reported that obese patients had a longer ICU and/or hospital stay [7–9, 11, 24–26, 28–31, 33] while four studies found no difference [12, 13, 28, 34, 35] and one study found a shorter duration of ICU and hospital stay in obese versus normal weight controls (Table 4) [10]. In our meta-analysis, there was little difference in duration of ICU and hospital length of stay for overweight and obese patients versus normal weight controls (Fig. 4). For both underweight and morbidly obese subjects versus normal weight subjects, there was a non-statistically significant trend toward longer mean ICU and hospital length of stays (underweight: 0.40 days, 95% CI, 0.01, 0.78 days and 1.39 days, 95% CI, –0.53, 2.67 days, respectively and morbid obesity: 0.77 days, 95% CI, −0.14, 2.03 days and 1.36 days, 95% CI, −2.08, 5.52 days, respectively). The sensitivity of our results (i.e., removing those studies without estimates of standard deviation) changed the pooled results for only morbidly obese patients such that there was a significant association with increased duration of ICU and hospital stay (1.2 days, 95% CI, 0.5, 2.2 days; and 2.9 days, 95% CI, 1.1, 4.3 days, respectively). For all comparisons, the I 2 statistic for heterogeneity was <40 and <13% for ICU stay and hospital stay, respectively, indicating consistency of results across studies and the utility of pooling the results across studies.
Forest plots showing the difference in mean days in the ICU and hospital comparing the underweight, overweight, obese and morbidly obese patients to the normal weight patients. For each comparison, we display the Bayesian pooled estimate with 95% credible intervals calculated maximum likelihood estimates
Other complications
The association of obesity with any other complications of critical illness was reported in only 7 of the 23 studies (Table 5). Neville [25] reported that obesity was associated with a higher risk for multi-organ failure while Brown et al. [26] found that the frequency of renal failure, deep venous thrombosis, multi-organ failure, and ARDS was higher in obese versus with non-obese patients. Higher rates of deep venous thrombosis and multi-organ failure, but not ARDS and renal failure, in obese versus non-obese patients were confirmed by these investigators in a subsequent investigation of patients with traumatic brain injury [29]. Ciesla et al. [30] found that obese trauma patients were more likely to develop multi-organ failure than non-obese patients after risk adjustment, but found not difference in the incidence of ARDS or renal failure. These existing studies have important limitations since the sample size was often small, the definition of ICU complications poorly defined, and only a non-obese control group (including underweight patients) was used.
Long term outcomes
Only 1 of 23 studies investigated patient outcomes after hospital discharge, reporting that obesity was associated with improved risk-adjusted survival at 1 year after critical illness [35]. The proportion of patients discharge to a secondary care facility was reported in only 3 of 23 studies [13, 24, 30]. Moreover, no data were reported regarding objective measures of ICU survivors’ physical function, mental health, or quality of life.
Discussion
In our meta-analysis of the impact of obesity in critical illness, we found that, compared with normal weight patients, obese and morbidly obese patients have no significant difference in ICU mortality, and obese patients may have lower hospital mortality. We found no significant association between obesity or morbid obesity with duration of mechanical ventilation, but morbid obesity may be associated with longer ICU and/or hospital stay. Importantly, we found very little research investigating the impact of obesity on patient outcomes after hospital discharge.
There are several explanations for a potential association between obesity and lower hospital mortality after critical illness including high levels of anti-inflammatory adipokines such as interleukin-10 and leptin that might positively modulate deleterious inflammatory processes [36]. High cholesterol and lipid levels common in obese patients might confer benefits during sepsis by binding endotoxins or by providing necessary precursors for adrenal steroid synthesis during acute illness [36]. Higher body weight has been further suggested to afford a nutritional reserve that becomes important for survival during acute life threatening illness [2]. Moreover, in some institutions, obese patients might be admitted to the ICU regardless of severity of illness given the need for higher nurse staffing not available elsewhere in the hospital. In a risk-adjusted cohort investigation, Bercault et al. [32] studied obese patient requiring mechanical ventilation >48 h. The risk of ICU mortality was double in the obese versus normal weight control group suggesting that, after considering severity of illness, obesity may be associated with mortality. Nonetheless, in studies that performed risk-adjusted analysis (Table 4), there were conflicting findings on whether obesity was independently associated with mortality after critical illness. Due to the marked variation in data reporting, we could not adjust for severity of illness in our meta-analysis.
Our results can be compared with the findings from the two other meta-analyses of obesity and mortality after critical illness. Akinnusi et al. [1] searched the literature up to February 2007 combining data from 14 studies with 62,045 patients. Consistent with our findings, these authors reported that obesity (BMI ≥30 kg/m2) was not associated with crude ICU mortality and that obese patients had lower hospital mortality than non-obese (BMI <30 kg/m2) patients (RR 0.83, 95% CI, 0.74, 0.92). However, they reported that in obese versus non-obese patients, there was a longer duration of mechanical ventilation (1.48 days, 95% CI, 0.07, 2.89,) and ICU length of stay (1.08 days, 95% CI, 0.27, 1.88). Oliveros et al. [2] pooled data from 12 of 23 studies that they identified in a literature search up to June 2007. Similar to our study, these authors compared mortality using a normal weight reference group (BMI 18.5–24.9 kg/m2). However, they did a combined analysis of ICU and hospital mortality and found a lower mortality for overweight (odds ratio 0.91, 95% CI, 0.84, 0.98) and obese (odds ratio 0.82, 95% CI, 0.68, 0.98), but not morbidly obese (OR 0.94, 0.82, 1.07) patients. Moreover, ICU length of stay was longer for underweight, overweight, and morbidly obese patients. In addition to separately examining ICU and hospital mortality, our study is distinguished from that of Oliveros et al. [2] by including the recently published 807 patient study by Smith et al. [19], and by combining operative and non-operative patients in the study by Finkielman et al. [8]. Furthermore, we excluded the studies by De Waele et al. [37] and Duane et al. [38] because we believed these studies were not limited to ICU outcomes. Finally, unlike this prior study, we excluded the 37,470 patient studied by Tremblay et al. [20] to prevent duplicate inclusion of the overlapping patient population with the 48,176 patient study by Marik et al. [7].
We were surprised that we did not find a relationship between obese patients and increased duration of mechanical ventilation. Obese patients are prone to atelectasis, aspiration, and pneumonia that may increase the duration of mechanical ventilation [5, 6]. Furthermore, obese patients have reduced lung and chest wall compliance leading to high airway resistance interfering with implementation of low airway pressure lung protective ventilation schemes for patients with acute lung injury (especially when ventilator settings are not based on ideal body weight) [23, 39]. Given the marked heterogeneity of the data and the lack of risk adjustment for potential differences in severity of illness between obese and normal-weight patients, the interpretation of the impact of obesity on duration of mechanical lung ventilation remains unresolved.
The improving mortality from critical illness is placing increasing emphasis on understanding the long-term outcomes of ICU survivors particularly since such patients might have physical and mental impairment and reduced quality of life after hospital discharge [15, 40–42]. Outside the context of critical illness, obesity is associated with high rates of disability, and functional impairment [4, 43–45]. Furthermore, obese individuals are reported to have higher levels of anxiety, depression, and lower scores for self-perceived health than non-obese subjects [46, 47]. With the exception of Peake et al. [35] who reported 1 year mortality, this review revealed the lack of data regarding the impact of obesity on outcomes after hospital discharge. Few studies evaluated whether obesity was related to need for nursing home placement or in-patient rehabilitation after critical illness [13, 24, 48]. Only one study evaluated whether obesity impacted functional outcome after hospital discharge, but the assessments were limited to whether a patient was independent, dependent, or deceased [20].
Although our analysis included over 80,000 patients, the varying definitions of obesity and heterogeneity among the included studies created limitations with conducting and interpretation the meta-analysis. We found substantial statistical heterogeneity within our analysis suggesting that a large degree of the differences in outcomes of obesity in the eligible studies might be explained by patient characteristics (other than BMI) across the studies. Most studies did not present risk-adjusted analyses of the association of BMI and duration of mechanical ventilation and ICU and hospital stay. Moreover, the meta-analysis could not consider any risk adjustment for differences in patient populations between the studies due to variation in the severity of illness scoring systems used and the lack of reporting of severity of illness data by BMI category. Moreover, we could not adjust for patient age in our analysis, an important limitation since obese patients tend to be younger than non-obese patients. Other limitations to the existing studies include high (>30% in some studies) or unknown rates of missing data, imprecise measurement of BMI (often estimated or based on patient-reported data), failure to account for the effects of fluid balance on body weight leading to “pseudo-obesity” in some subjects, varying definitions of outcomes, and incompletely defined control groups.
In conclusion, our meta-analysis of studies evaluating the effect of obesity in critical illness suggests that obesity and morbid obesity does not adversely impact ICU mortality. Obesity may be associated with lower hospital mortality compared with normal body weight. Obesity was not associated with the duration of mechanical ventilation or ICU or hospital length of stay. However, morbid obesity may be associated with longer ICU and hospital length of stay. There is a critical deficiency of data on the influence of obesity on complications of critical illness and patient outcomes after hospital discharge. Given that obesity is common, costly, and associated with substantial morbidity and mortality in the general population, efforts to understand the impact of obesity on ICU care, complications and long-term outcomes after critical illness should be a research priority.
References
Akinnusi M, Pineda L, El Solh A (2008) Effect of obesity on intensive care morbidity and mortality: a meta-analysis. Crit Care Med 36:151–158
Oliveros H, Villamor E (2008) Obesity and mortality in critically ill adults: a systematic review and meta-analysis. Obesity 16:515–521
Thompson D, Eldesberg J, Colditz G, Bird A, Oster G (1999) Lifetime health and economic consequences of obesity. Arch Intern Med 159:2177–2183
Flegal K, Graubard B, Williamson D, Gail M (2005) Excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc 293:1861–1867
Pieracci F, Barie P, Pomp A (2006) Critical care of the bariatric patient. Crit Care Med 34:1796–1804
Ebert T, Shankar H, Haake R (2006) Perioperative considerations for patients with morbid obesity. Anesth Clin North Am 24:621–636
Marik P, Doyle H, Varon J (2003) Is obesity protective during critical illness? An analysis of a National ICU database. Crit Care Shock 6:156–162
Finkielman J, Gajic O, Afessa B (2004) Underweight is independently associated with mortality in post-operative and non-operative patients admitted to the intensive care unit: a retrospective study. BMC Emerg Med 4:1–7
Garrouste-Orgeas M, Troché G, Azoulay E, Caubel A, de Lassence A, Cheval C, Montesino L, Thuong M, Vincent F, Cohen Y, Timsit J (2004) Body mass index. An additional prognostic factor in ICU patients. Intensive Care Med 30:437–443
Nasraway S Jr, Albert M, Donnelly A, Ruthazer R, Shikora S, Saltzman E (2006) Morbid obesity is an independent determinant of death among surgical critical ill patients. Crit Care Med 34:964–970
Bochicchio G, Joshi M, Bochicchio K, Nehman S, Tracy J, Scalea T (2006) Impact of obesity in the critically ill trauma patient: a prospective study. J Am Coll Surg 203
Aldawood A, Arabi Y, Dabbagh O (2006) Association of obesity with increased mortality in the critically ill patient. Anaesth Intensive Care 34:629–633
O’Brien J Jr, Phillips G, Ali N, Lucarelli M, Marsh C, Lemeshow S (2006) Body mass index is not independently associated with hospital mortality in mechanically ventilated adults with acute lung injury. Crit Care Med 34:738–744
Milberg J, Davis D, Steinberg K, Hudson L (1995) Improved survival of patients with acute respiratory distress syndrome (ARDS): 1983–1993. J Am Med Assoc 273:306–309
Cheung A, Tansey C, Tomlinson G, Diaz-Granados N, Matté A, Barr A, Mehta S, Mazer C, Guest C, Stewart T, Al-Saidi F, Cooper A, Cook D, Slutsky A, MS H (2006) Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 174:538–544
Hopkins R, Weaver L, Collingridge D, Parkinson R, Chan K, Orme J Jr (2005) Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med 171:340–347
Wells G, O’Connell D, Peterson J, Welch V, Tugwell P (2000) The Newcastle-Ottawa scale for re-assessing the quality of nonrandomised studies in meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
Stevens R, Dowdy D, Michaels R, Mendez-Tellez P, Pronovost P, Needham D (2007) Neuromuscular dysfunction acquired in critical illness: a systematic review. Int Care Med 33:1876–1891
Smith R, Chong T, Hedrick T, Hughes M, Evans H, McElearney S, Pruett T, Sawyer R (2007) Does body mass index affect infection-related outcomes in the intensive care unit? Surg Infect 8:581–588
Tremblay A, Bandi V (2003) Impact of body mass index on outcomes following critical care. Chest 123:1202–1207
Newell M, Bard M, Goettler C, Toschlog E, Schenarts P, Sagraves S, Holbert D, Pories W, Rotondo M (2007) Body mass index and outcomes in critically injured blunt trauma patients: weighing the impact. J Am Coll Surg 204:1056–1064
Higgins J, Thompson S (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558
O’Brien J Jr, Welsh C, Fish R, Ancukiewicz M, Kramer A, National Heart L, and Blood Institute Acute Respiratory Distress Syndrome Network (2004) Excess body weight is not independently associated with outcome in mechanically ventilated patients with acute lung injury. Ann Intern Med 140:338–345
Morris A, Stapleton R, Rubenfeld G, Hudson L, Caldwell E, Steinberg K (2007) The association between body mass index and clinical outcomes in acute lung injury. Chest 131:342–348
Neville A, Brown C, Weng J, Demetriades D, Velmahos G (2004) Obesity is an independent risk factor of mortality in severely injured blunt trauma patients. Arch Surg 139:983–987
Brown C, Neville A, Rhee P, Salim A, Velmahos G, Demetriades D (2005) The impact of obesity on the outcomes of 1,153 critically injured blunt trauma patients. J Trauma 59:1048–1051
Byrnes M, McDaniel M, Moore M, Helmer S, Smith R (2005) The effect of obesity on outcomes among injured patients. J Trauma 58:232–237
Alban R, Lyass S, Margulies D, Shabot M (2006) Obesity does not affect mortality after trauma. Am Surg 10:966–969
Brown C, Rhee P, Neville A, Sangthong B, Salim A, Demetriades D (2006) Obesity and traumatic brain injury. J Trauma 61:572–576
Ciesla D, Moore E, Johnson J, Burch J, Cothren C, Sauaia A (2006) Obesity increases risk for organ failure after severe trauma. J Am Coll Surg 203:539–545
El-Solh A, Sikka P, Bozkanat E, Jaafar W, Davies J (2001) Morbid obesity in the medical ICU. Chest 120:1989–1997
Bercault N, Boulain T, Kuteifan K, Wolf M, Runge I, Fleury J (2004) Obesity-related excess mortality rate in an adult intensive care unit: a risk-adjusted matched cohort study. Crit Care Med 32:998–1003
Goulenok C, Monchi M, Chiche J, Mira J, Dhainaut J, Cariou A (2004) Influence of overweight on ICU mortality. Chest 125:1441–1445
Ray D, Matchett S, Baker K, Wasser T, Young M (2005) The effect of body mass index on patient outcomes in a medical ICU. Chest 127:2125–2131
Peake S, Moran J, Ghelani D, Lloyd A, Walker M (2006) The effect of obesity on 12-month survival following admission to intensive care: a prospective study. Crit Care Med 34:2929–2939
Rice T (2007) Obesity in acute lung injury: the “weight” is over. Chest 131:333–334
De Waele B, Vanmierlo B, Van Nieuwenhove Y, Delvaux G (2006) Impact of body overweight and class I, II, and III obesity on the outcome of acute biliary pancreatitis. Pancreas 32:343–345
Duane T, Dechert T, Aboutanos M, Malhotra A, Ivatury R (2006) Obesity and outcomes after blunt trauma. J Trauma 61:1218–1221
Fan E, Needham D, Stewart T (2005) Ventilatory management of acute lung injury and acute respiratory distress syndrome. J Am Med Assoc 294:2889–2896
Bernard G (2005) Acute respiratory distress syndrome: a historical perspective. Am J Respir Crit Care Med 172:798–806
Hopkins R, Weaver L, Chan K, Orme JJ (2004) Quality of life, emotional, and cognitive function following acute respiratory distress syndrome. J Int Neuropsychol Soc 10:1005–1017
Heyland D, Groll D, Caeser M (2005) Survivors of acute respiratory distress syndrome: relationship between pulmonary dysfunction and long-term health-related quality of life. Crit Care Med 33:1549–1556
Gregg E, Cheng Y, Cadwell B, Imperatore G, Williams D, Flegal K, Narayan K, Willisamson D (2005) Secular trends in cardiovascular disease risk factors according to body mass index in US adults. J Am Med Assoc 293:1868–1874
Allley D, Chang V (2007) The changing relationship of obesity and disability, 1988–2004. J Am Med Assoc 298:2020–2027
Mokdad A, Ford E, Bowman B, Dietz W, Vinicor F, Bales V, Marks J (2003) Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. J Am Med Assoc 289:76–79
Sullivan M, Karlsson J, Sjöström L, Backman L, Bengtsson C, Bouchard C, Dahlgren S, Jonsson E, Larsson B, Lindstedt S (1993) Swedish obese subjects (SOS)—an intervention study of obesity. Baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes Relat Metab Disord 17:503–512
Doll H, Petersen S, Stewart-Brown S (2000) Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res 8:160–170
Yaegashi M, Raymonde J, Zuriqat M, Noack S, Homel P (2005) Outcome of morbid obesity in the intensive care unit. J Int Care Med 20:147–154
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hogue, C.W., Stearns, J.D., Colantuoni, E. et al. The impact of obesity on outcomes after critical illness: a meta-analysis. Intensive Care Med 35, 1152–1170 (2009). https://doi.org/10.1007/s00134-009-1424-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-009-1424-5