Abstract
Objective
Compared to oronasal interfaces, a cephalic mask has a larger inner volume, covers the entire anterior surface of the face and limits the risk of deleterious cutaneous side effects during noninvasive ventilation (NIV). The present clinical study aimed to compare the clinical efficacy of a cephalic mask versus an oronasal mask in patients with acute hypercapnic respiratory failure (AHRF).
Design and setting
Randomized controlled study in a Respiratory Intermediate Care Unit.
Patients
All consecutive patients admitted for AHRF were randomly assigned to receive bilevel NIV either with a cephalic mask (n = 17) or an oronasal mask (n = 17) during the first 48 h.
Measurements
The main outcome criterion was the improvement of arterial pH, 24 h after NIV initiation. Secondary criteria included PaCO2 and physiological parameters.
Results
Compared to values at inclusion, pH, PaCO2, encephalopathy score, respiratory distress score and respiratory frequency improved significantly and similarly with both masks. None of these parameters showed statistically significant differences between the masks at each time point throughout the study period. Mean delivered inspiratory and expiratory pressures were similar in both patient groups. Tolerance of the oronasal mask was improved at 24 h and further. One patient with the cephalic mask suffered from claustrophobia that did not lead to premature study interruption.
Conclusions
In spite of its larger inner volume, the cephalic mask has the same clinical efficacy and requires the same ventilatory settings as the oronasal mask during AHRF.
Similar content being viewed by others
Introduction
Noninvasive ventilation (NIV) reduces the work of breathing [1], the need for endotracheal intubation [2–6], the duration of hospitalization [7], mortality rates [7, 8] and the incidence of complications [7] in COPD patients with acute hypercapnic respiratory failure (AHRF). Clinical studies are still necessary to determine why NIV fails in approximately 20–30% of these patients [6–10] and in an even higher percentage of patients with restrictive pulmonary disorders and AHRF [11]. In an observational cohort study of non-selected patients, Girault et al. found that NIV failures during various aetiologies of AHRF ranged from 35 to 49% [12]. This rather high failure rate may be due to clinical [1, 10, 13, 14] or technical factors such as ventilatory modes and ventilatory settings [6, 15]. Finally, poor adaptation to the nasal/oronasal interfaces may lead to asynchrony, to unintentional leaks and may also be responsible for some cases of NIV failure [16, 17].
While physiological studies comparing different patient-ventilator interfaces have been performed [18–21], very few clinical studies have compared their efficacy and tolerance during AHRF [16, 22–24]. Oronasal masks have been associated with deleterious consequences such as gas leaks around the mask, skin breakdown, claustrophobia and discomfort [25]. In order to limit these side effects, new interfaces such as the cephalic mask [18] and helmet [16] have recently been developed, but clinical experience with these devices is still limited. The cephalic mask covers the entire anterior surface of the face [18]. Mask-fit pressure is therefore spread over a larger surface beyond the nose area, limiting the risk of deleterious cutaneous side effects.
The cephalic mask has a large inner volume and therefore a larger anatomical dead space that may interfere with clinical NIV efficacy and patient-ventilator interaction. However, in a lung model study, Saatci et al. [21] have shown that its dynamic dead space is not that much larger when compared to an oronasal mask, probably because of exhalation ports located on the mask and possibly also because of stagnant air within the mask that does not contribute to rebreathing. From the bench model study of Saatci et al., we may assume that a cephalic mask is as effective as an oronasal mask but this remains to be proven in clinical settings. Our study was therefore designed to assess the clinical efficacy of the cephalic mask versus a conventional oronasal mask for managing patients with AHRF.
Patients and methods
Patients
Thirty-four consecutive patients hospitalized in our Respiratory Intermediate Care Unit (RICU) for AHRF were prospectively included in the study. The study protocol was approved by the institutional review board of Rouen University Hospital. Written informed consent was obtained from all the patients or a member of their family. Inclusion criteria were AHRF as defined as an arterial pH ≤ 7.35 and a PaCO2 ≥ 6.5 kPa, the absence of immediate criteria for endotracheal intubation and randomization within two hours of admission to the RICU. Exclusion criteria were AHRF secondary to pneumothorax or suspected pulmonary embolism (based on high clinical probability), absence of patient cooperation, facial abnormalities precluding NIV, previously known ophthalmologic diseases and previous home ventilation using a cephalic or oronasal mask. Endotracheal intubation was performed in patients with one major or two minor criteria according to Brochard et al. [7]. The major criteria included respiratory arrest, gasping, coma, agitation requiring sedation, heart rate <50/min with unconsciousness and haemodynamic instability with systolic arterial pressure <70 mmHg. The minor criteria were respiratory rate >35/min and above the rate at admission, PaO2 <6 kPa despite oxygen therapy and alteration of the encephalopathy score. The same criteria were used when endotracheal intubation was considered throughout the study period.
Masks
Patients were randomized to ventilate either with a cephalic (C) mask (Total Face, Respironics, Pittsburgh, PA) or with a conventional facial (F) mask (ComfortFull, Respironics). The C mask covers the mouth, eyes and nose and is maintained in place by two Velcro strips attached at the back of the head. A soft silicone layer ensures air tightness. This mask has two intentional leaks in front of the mouth. The C mask is only available in one size and is equipped with a safety valve that opens in case of unexpected ventilator failure. We measured the mask volumes by filling the interfaces with water. The volume of water was assessed before and after introducing a mannequin face inside the interface. We determined that the inner volume of the C mask, less the volume of water displaced by the mannequin face, was 900 mL. A recent physiological study reported a slightly higher value of 967 mL [21]. According to the manufacturer, airflow through the intentional leaks varies from 24.7 L/min at a positive inspiratory pressure (PIP) of 5 mbar to 48.3 L/min for a PIP of 20 mbar.
The F mask is an oronasal mask that incorporates intentional leaks at the junction with the circuit and is equipped with a safety valve as in the C mask. It has a silicone cushion and four attachment points for the headgear to the harness. We determined that the inner volume of the F mask, less the volume of water displaced by the mannequin face, was 240–375 mL, depending on the size (small, medium, large) of the mask. According to the manufacturer, airflow through the intentional leaks varies from 20.0 L/min at a PIP of 5 mbar to 42 L/min for a PIP of 20 mbar. The intentional leaks are always lower with the F mask than the C mask, whatever the PIP value.
Study design
This prospective randomized controlled study was equipped with an equivalence hypothesis. The main outcome criterion was the improvement of arterial pH, 24 h after NIV initiation. The secondary outcome criteria were: improvement of arterial PCO2, endotracheal intubation rates, hospital mortality, respiratory rate, distress score, encephalopathy score, Glasgow score, adaptation to NIV (patient-ventilator adaptation) and mask tolerance as judged by the patient, RICU length of stay and hospital length of stay. The study was terminated if there was a need to change the mask or ventilatory mode or in the event of death or endotracheal intubation.
Follow-up was assessed by clinical evaluation, respiratory rate and arterial blood gas levels at 1, 2, 12, 24 and 48 h after initiation of NIV. Respiratory distress was evaluated from the use of accessory muscles and scored from 0 to 5 according to Patrick et al. [26]. The encephalopathy score was the sum of flapping tremor, confusion, somnolence and agitation rated from 0 (absent) to 1 (mild) or 2 (moderate to severe). Patient-ventilator adaptation (i.e. patient-ventilator interaction based on synchronization and pressurization), was assessed by the respiratory physician on duty and rated from 0 (null) to 4 (optimal). Subjective tolerance of the mask (defined as the ability to endure the mask) was evaluated by the following question: “How do you tolerate this mask?” and the patient was asked to rate his sensation using the verbal scale with a lower limit at 0 (not tolerated at all) and an upper limit at 5 (very well tolerated). The Glasgow score was recorded at each time period. The following adverse events were recorded throughout the study period: facial skin necrosis, conjunctivitis, gastric distension, aspiration and claustrophobia associated with the interface.
We used domiciliary bilevel ventilators in pressure support mode with a fixed back-up rate of 12/min. Inspiratory pressure was initially set at 12 mbar and thereafter increased in order to optimize patient-ventilator interaction. PEEP was increased from 4 mbar according to synchronization and hypoxaemia. Inspiratory triggers were set at the most sensitive level allowed by the ventilator and, if necessary, modified in order to optimize synchronization and to eliminate autotriggering. Expiratory cycling was first set at the “automatic” value displayed by these ventilators or at 25% of peak inspiratory flow and secondarily modified in order to optimize synchronization. Heart rate, non-invasive blood pressure and SpO2 were continuously monitored. FIO2 was set to provide a SpO2 ≥90% and regularly checked with an oxygen sensor (Oxy 2100, CFPO, France). In parallel with NIV, all patients were administered standard medical therapy and respiratory care as prescribed by the physician on duty. Patients were instructed to use the ventilator as much as possible during the first day and air leakage around the mask was regularly evaluated and corrected by the RICU staff. In our RICU, all the nurses and respiratory therapists are specifically trained in NIV and a dedicated senior respiratory physician is on call 24 h a day.
Statistical analysis
Randomization assignment to the C or the F-groups was performed using the envelope technique. Continuous variables were expressed as means ± standard deviation unless otherwise mentioned. Statistical differences between discontinuous variables were assessed by the Fisher exact test. Differences between continuous variables were assessed by the Mann–Whitney test. Evolution in pH, PaCO2 and respiratory frequency at each time point were analyzed using a two-way ANOVA. Evolution in clinical scores was analyzed by the Friedman test and comparisons between groups at each time point were performed using the Mann–Whitney test. All statistical analyses were performed on an intention-to-treat basis that applied to all the patients. The equivalence of the masks was defined by an arterial pH difference of less than 0.05 after 24 h of NIV. The sample size was calculated with nQuery software (Statistical Solutions, Saugus, MA). For an equivalence hypothesis, 28 patients are needed for a study power of 80% and an alpha significance level of 0.05. The statistical analyses were performed using SAS 8.02 software (SAS Institute, Cary, NC).
Results
Patients
Seventeen patients were ventilated with the C mask and 17 patients with the F mask. Baseline clinical characteristics (Table 1), pulmonary function tests and arterial blood gas levels during the 6 months before inclusion (Table 2) were similar in both groups. A high proportion of patients had COPD (82% in the C group and 76% in the F group). A similar proportion of patients in both groups had been previously treated with home NIV, exclusively with a nasal mask. Severity at inclusion and the triggering factors for AHRF were similar in both groups (Table 3).
Patients in the C group were ventilated with the following ventilators: Breas PV102 (n = 3), Saime VS Integra (n = 5), Harmony (n = 1), Smartair Airox (n = 7) and Knightstar 330 (n = 1) barometric ventilators. Patients in the F group used Breas PV102 (n = 4), Saime VS Integra (n = 4), Harmony (n = 1), Airox Smartair (n = 6), and ResMed VPAP III STA (n = 2) barometric ventilators.
Evolution of arterial blood gases
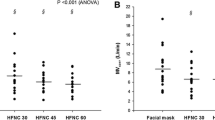
Compared to values at inclusion, pH under NIV improved significantly with both the C and F masks (p < 0.0001, Fig. 1a). pH was significantly improved at H1 with the C mask (p = 0.0365) and at H12 with the F mask (p = 0.0066). There were no statistically significant differences between the masks at any study period. When measured under spontaneous breathing at H24 and H48, pH at H24 had improved from the values at inclusion with both the C (p = 0.0013) and the F masks (p = 0.0003). Inter-value comparisons using the Mann-Whitney test did not reveal any significant differences between the masks at inclusion, H24 and H48.
Evolution of arterial pH and PCO2 under NIV. a pH improved significantly at H1 with the C mask, (p = 0.0365) and at H12 with the F mask (p = 0.0066). There were no significant differences between the masks throughout the study period. b PaCO2 under NIV improved slightly faster with the C mask (statistical significance at H12 with the C mask vs. H48 with the F mask), but there were no statistically significant differences between the masks throughout the study period
PaCO2 under NIV improved significantly from inclusion with both the C (p < 0.0026) and F masks (p < 0.0028) but slightly faster with the C mask (significant at H12 with the C mask vs. H48 with the F mask, Fig. 1b). There were no statistically significant differences in terms of PaCO2 between the masks throughout the study period. Under spontaneous breathing at H24 and H48, PaCO2 had improved significantly at H24 with the C mask (p = 0.0083) but only at H48 with the F mask (p = 0.0165) relative to inclusion values. Inter-value comparisons using the Mann–Whitney test did not reveal any significant differences between the masks at inclusion, H24 or H48.
Encephalopathy scores, distress scores and respiratory rates
ANOVA analyses showed that encephalopathy scores improved significantly with both the C (p < 0.0001) and F masks (p < 0.0113, Fig. 2) relative to inclusion values and these improvements became significant from H12 for both the C (p = 0.0007) and F masks (p = 0.0147). Similarly, distress scores and respiratory rates under NIV improved significantly with both the C (p < 0.0001) and the F masks (p < 0.0001, Fig. 2) relative to values at inclusion. Distress scores improved significantly at H1 with the C mask (p = 0.0380) and at H2 with the F mask (p = 0.0224). Respiratory rate under NIV improved significantly at H12 with the C mask (p = 0.0014) and at H2 with the F mask (p = 0.0092). Comparisons using the Mann–Whitney test did not reveal any significant differences between the masks for any of these three parameters at any study period. Finally, respiratory rate under spontaneous breathing improved significantly at H24 and H48 with both masks.
Evolution of clinical parameters under NIV. Encephalopathy scores (a), respiratory distress scores (b) and respiratory rate under NIV (c) improved significantly with both the C and F masks relative to inclusion values. For all parameters, there were no statistically significant differences between the masks throughout the study period
Outcome
In the F group, the study was interrupted in two patients who refused to wear the mask. Moreover, in the same group, one patient died of pneumonia at H2 after having refused intubation (Table 4). In the C group, one patient was intubated and died of pneumonia at H12; the study was interrupted in another patient because of mask intolerance. Intubation rates and premature study interruption were statistically similar in both groups.
Mean PIP values were similar in patients ventilated with the C mask (21.1 ± 2.6 mbar) and the F mask (20.7 ± 1.6 mbar). Mean PEEP values were also similar in the C group (5.7 ± 1.8 mbar) and the F group (5.1 ± 1.6 mbar). During the first 24 h, the mean duration of NIV was 13.7 ± 3.3 h with the C mask and 14.1 ± 2.8 h with the F mask. Throughout the 48 h of the study, the mean duration of NIV was 25.3 ± 2.1 h with the C mask and 26.4 ± 3.0 h with the F mask. These differences were not statistically significant.
The mean lengths of stay (LOS) in RICU and in hospital were similar in both groups (Table 4). The median (interquartile range) LOS in RICU were similar with the C mask [10 days (7–14.5)] and the F mask [10 days (6.75–16.5)]. The median LOS in hospital were also similar with the C mask [13 days (10.25–17.25] and the F mask [17 days (13.5–21)].
Complications, tolerance and adaptation scores
Two complications associated with the F mask were noted during the 48-h study period (Table 4). One patient developed conjunctivitis and another developed gastric distension. One patient with the C mask suffered from claustrophobia. None of these complications led to premature study interruption.
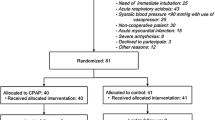
Analysis using the Friedman test did not reveal any significant changes in adaptation score during the 48 h for both the C (p = 0.8836) and F masks (p = 0.5548, Fig. 3a). An inter-group analysis using the Mann–Whitney test did not reveal any statistically significant difference in adaptation to NIV with either mask at any time during the study period. Tolerance score significantly improved with the F mask during the 48 h (p = 0.0006) but not with the C mask (p = 0.9053). Inter-group analysis revealed that both masks were equally tolerated by the patients during the first 24 h of the study but tolerance was significantly better with the F mask than with the C mask at H24 (p = 0.0328) and H48 (p = 0.0298) (Fig. 3b).
Evolution of adaptation and tolerance scores under NIV. ANOVA analyses did not reveal any significant changes in adaptation scores (a) with either mask during the first 48 h. Tolerance scores (b) were similar with either mask during the first 24 h of the study but tolerance was better with the F mask from H24 to H48
Discussion
The main findings of the present study are the following: (1) the C mask was clinically as effective as the F mask in managing patients with AHRF, (2) the larger inner volume of the C mask did not interfere with clinical efficacy and (3) this larger inner volume did not require modification of PIP or PEEP, at least compared with the F mask. In order to assess the clinical efficacy of the C mask, the F mask was chosen as the comparator because this conventional oronasal mask is regularly used in our RICU and can therefore be considered as a reference interface in our hands. We compared the clinical efficacy of both interfaces using arterial blood gas values as the main outcome criteria. Arterial blood gases are major criteria used to assess outcome under NIV during AHRF and our study was sufficiently powered to correctly interpret these criteria. Using intubation rate or NIV success as the main criterion would have required a very large sample size.
Only a few randomized clinical studies have compared the clinical efficacy of different interfaces during NIV. In 26 patients with different causes of chronic hypercapnic respiratory failure in a stable state, Navalesi et al. [23] found that oronasal masks were more effective in improving arterial blood gas levels and minute ventilation but that nasal masks were better tolerated. In a study involving 16 stable patients with sleep disordered breathing and daytime hypercapnia, Willson et al. [27] reported that nasal masks were as effective as oronasal masks in improving nocturnal hypoventilation and tended to be more comfortable. In the context of acute respiratory failure with or without hypercapnia treated either with bilevel or CPAP ventilation, Kwok et al. [22] reported that oronasal masks were as efficient (i.e. similar intubation rate, PaCO2 evolution, NIV duration, hospital duration and mortality) but were better tolerated than nasal masks. Finally, claustrophobia was mentioned more frequently with the oronasal mask but was not considered to be true intolerance and did not lead to NIV failure. The only clinical study on the cephalic mask was reported by Criner et al. [18], who found that a prototype was as efficient as nasal and oronasal masks in order to improve blood gases in hypercapnic patients with chronic respiratory failure. Their patients did not complain of discomfort with the cephalic mask and reported limited side effects. Conversely, our study was performed in patients hospitalized in RICU with AHRF. The cephalic mask was associated with good clinical efficacy and its tolerance was not modified throughout the 48-h study period. We observed that the F mask was better tolerated after the first 24 h, perhaps because this type of interface was more familiar to the included patients using NIV at home. However, a verbal scale is an imperfect method to assess their impression of tolerance and our sample size may not have been sufficiently powered to appreciate inter-patient variability of this parameter. Our results concerning tolerance are mainly a rationale for a dedicated study that would assess tolerance of the C mask as a primary outcome criterion.
In addition to clinical comparisons, researchers have recently addressed the issue of physiological interface behaviour, especially in relation to inner mask volume, effective dead space volume and CO2 rebreathing during NIV. Schettino et al. [20] have demonstrated that the location of exhalation ports on the mask surface is a more relevant factor in limiting CO2 rebreathing than the inner volume of the interface per se [20]. In a lung model study, Saatci et al. [21] confirmed that inner mask volume (especially cephalic masks), bears little relation to the dynamic dead space when connected to the ventilator. The behaviour of physiological dead space is mainly related to the presence of positive pressure throughout the expiratory phase [21] and consequently to the level of flow through the exhalation ports. It is also probably related to complex air dynamics inside the mask [21] (a phenomenon that is still not completely understood) and to the location of the exhalation ports [20], near the nasal bridge, at cheek level or on the circuit. The results of our clinical study are in accordance with these previous physiological data. Indeed, we found a clinical equivalence between the cephalic and the oronasal mask, in accordance with their roughly similar dynamic dead spaces as pointed out by Saatci et al. [21]. Of clinical importance, we also found that the cephalic interface did not require different PIP or PEEP settings from those used with the oronasal mask.
One limitation of our study was that some of our patients had been previously treated with home NIV. However, we included these patients in our analysis because none of them were ventilated at home with a cephalic or an oronasal mask. In addition, there were similar proportions of these patients in the F and C groups. Another limitation was that several ventilators were used in this study. Because the cephalic mask incorporates exhalation ports on its surface, this interface can only be used with turbine-driven ventilators and single-branch circuits. We used domiciliary ventilators, which are commonly used in RICUs or in some Emergency Care Units, but the performances of these ventilators may be different, particularly in presence of air leaks [28, 29]. This last issue has not been addressed with domiciliary ventilators and its clinical relevance and impact on comfort and tolerance still need to be evaluated. We think that progressive setting of inspiratory and expiratory cycling as performed in this study (and routinely in our RICU), was a way to optimize the capacities of each ventilator used in these patients. Finally, because our study was a clinical study, it was not possible to strictly consider that both patient arms only differed by their interfaces. When assessing interfaces or ventilatory parameters during NIV, it is extremely difficult (and almost impossible) to vary only one parameter in order to evaluate its impact. This difficulty may be partially circumvented by developing bench test studies, where many parameters may be fixed. In spite of this, we think that clinical evaluations like our study can provide pertinent information for physicians, especially when they are performed by trained staff with patients presenting representative aetiologies of AHRF.
In conclusion, the cephalic mask has the same clinical efficacy as the oronasal mask during AHRF. In spite of a larger inner volume, the cephalic interface does not require modification of ventilatory settings and may be a satisfactory alternative to oronasal masks.
References
British Thoracic Society (2002) Non-invasive ventilation in acute respiratory failure. Thorax 57:192–211
Brochard L, Isabey D, Piquet J, Amaro P, Mancebo J, Messadi AA, Brun-Buisson C, Rauss A, Lemaire F, Harf A (1990) Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med 323:1523–1530
Meduri GU (1996) Noninvasive positive-pressure ventilation in patients with acute respiratory failure. Clin Chest Med 17:513–553
Vitacca M, Clini E, Rubini F, Nava S, Foglio K, Ambrosino N (1996) Non-invasive mechanical ventilation in severe chronic obstructive lung disease and acute respiratory failure: short- and long-term prognosis. Intensive Care Med 22:94–100
Hilbert G, Gruson D, Gbikpi-Benissan G, Cardinaud JP (1997) Sequential use of noninvasive pressure support ventilation for acute exacerbations of COPD. Intensive Care Med 23:955–961
Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS (1995) Randomized prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 151:1799–1806
Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simonneau G, Benito S, Gasparetto A, Lemaire F (1995) Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med 333:817–822
Bott J, Carroll MP, Conway JH, Keilty SE, Ward EM, Brown AM, Paul EA, Elliott MW, Godfrey RC, Wedzicha JA, Moxham J (1993) Randomised controlled trial of nasal ventilation in acute ventilatory failure due to chronic obstructive airways disease. Lancet 341:1555–1557
Celikel T, Sungur M, Ceyhan B, Karakurt S (1998) Comparison of noninvasive positive pressure ventilation with standard medical therapy in hypercapnic acute respiratory failure. Chest 114:1636–1642
Plant PK, Owen JL, Elliott MW (2000) Early use of non-invasive ventilation for acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicentre randomised controlled trial. Lancet 355:1931–1935
Robino C, Faisy C, Diehl JL, Rezgui N, Labrousse J, Guerot E (2003) Effectiveness of non-invasive positive pressure ventilation differs between decompensated chronic restrictive and obstructive pulmonary disease patients. Intensive Care Med 29:603–610
Girault C, Briel A, Hellot MF, Tamion F, Woinet D, Leroy J, Bonmarchand G (2003) Noninvasive mechanical ventilation in clinical practice: a 2-year experience in a medical intensive care unit. Crit Care Med 31:552–559
Ambrosino N, Foglio K, Rubini F, Clini E, Nava S, Vitacca M (1995) Non-invasive mechanical ventilation in acute respiratory failure due to chronic obstructive pulmonary disease: correlates for success. Thorax 50:755–757
Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L (2001) Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med 163:874–880
Cuvelier A, Muir JF (2005) Technical practices are important to consider when assessing noninvasive ventilation failure. Eur Respir J 25:1130–1131
Antonelli M, Pennisi MA, Pelosi P, Gregoretti C, Squadrone V, Rocco M, Cecchini L, Chiumello D, Severgnini P, Proietti R, Navalesi P, Conti G (2004) Noninvasive positive pressure ventilation using a helmet in patients with acute exacerbation of chronic obstructive pulmonary disease: a feasibility study. Anesthesiology 100:16–24
Elliott MW (2004) The interface: crucial for successful noninvasive ventilation. Eur Respir J 23:7–8
Criner GJ, Travaline JM, Brennan KJ, Kreimer DT (1994) Efficacy of a new full face mask for noninvasive positive pressure ventilation. Chest 106:1109–1115
Chiumello D, Pelosi P, Carlesso E, Severgnini P, Aspesi M, Gamberoni C, Antonelli M, Conti G, Chiaranda M, Gattinoni L (2003) Noninvasive positive pressure ventilation delivered by helmet vs. standard face mask. Intensive Care Med 29:1671–1679
Schettino GP, Chatmongkolchart S, Hess DR, Kacmarek RM (2003) Position of exhalation port and mask design affect CO2 rebreathing during noninvasive positive pressure ventilation. Crit Care Med 31:2178–2182
Saatci E, Miller DM, Stell IM, Lee KC, Moxham J (2004) Dynamic dead space in face masks used with noninvasive ventilators: a lung model study. Eur Respir J 23:129–135
Kwok H, McCormack J, Cece R, Houtchens J, Hill NS (2003) Controlled trial of oronasal versus nasal mask ventilation in the treatment of acute respiratory failure. Crit Care Med 31:468–473
Navalesi P, Fanfulla F, Frigerio P, Gregoretti C, Nava S (2000) Physiologic evaluation of noninvasive mechanical ventilation delivered with three types of masks in patients with chronic hypercapnic respiratory failure. Crit Care Med 28:1785–1790
Anton A, Tarrega J, Giner J, Guell R, Sanchis J (2003) Acute physiologic effects of nasal and full-face masks during noninvasive positive-pressure ventilation in patients with acute exacerbations of chronic obstructive pulmonary disease. Respir Care 48:922–925
Gregoretti C, Confalonieri M, Navalesi P, Squadrone V, Frigerio P, Beltrame F, Carbone G, Conti G, Gamna F, Nava S, Calderini E, Skrobik Y, Antonelli M (2002) Evaluation of patient skin breakdown and comfort with a new face mask for non-invasive ventilation: a multi-center study. Intensive Care Med 28:278–284
Patrick W, Webster K, Ludwig L, Roberts D, Wiebe P, Younes M (1996) Noninvasive positive-pressure ventilation in acute respiratory distress without prior chronic respiratory failure. Am J Respir Crit Care Med 153:1005–1011
Willson GN, Piper AJ, Norman M, Chaseling WG, Milross MA, Collins ER, Grunstein RR (2004) Nasal versus full face mask for noninvasive ventilation in chronic respiratory failure. Eur Respir J 23:605–609
Miyoshi E, Fujino Y, Uchiyama A, Mashimo T, Nishimura M (2005) Effects of gas leak on triggering function, humidification, and inspiratory oxygen fraction during noninvasive positive airway pressure ventilation. Chest 128:3691–3698
Vignaux L, Tassaux D, Jolliet P (2007) Performance of noninvasive ventilation modes on ICU ventilators during pressure support: a bench model study. Intensive Care Med 33:1444–1451
Acknowledgments
The authors are grateful to François Dugardin and Dominique Métayer (Fédération ANTADIR) for their technical assistance and to Richard Medeiros (Rouen University Hospital Medical Editor) and Marilyn Amouyal-Jones for their editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuvelier, A., Pujol, W., Pramil, S. et al. Cephalic versus oronasal mask for noninvasive ventilation in acute hypercapnic respiratory failure. Intensive Care Med 35, 519–526 (2009). https://doi.org/10.1007/s00134-008-1327-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-008-1327-x