Abstract
Objective
Multiple-site colonization with Candida species is commonly recognized as a major risk factor for invasive fungal infection in critically ill patients. The fungal colonization density could be of predictive value for the diagnosis of systemic candidiasis in high-risk surgical patients. Little is known about it in the medical ICU setting.
Design and setting
Prospective observational study in the eight-bed medical intensive care unit of a teaching hospital.
Subjects
92 consecutive nonneutropenic patients hospitalized for more than 7 days.
Measurements and results
The colonization index (ratio of the number of culture-positive surveillance sites for Candida spp. to the number of sites cultured) was calculated weekly upon ICU admission until death or discharge. The 0.50 threshold was reached in 36 (39.1%) patients, almost exclusively in those with detectable fungal colonization upon ICU admission. The duration of broad-spectrum antibiotic therapy was found to be the main factor that independently promoted fungal growth as measured through the colonization index.
Conclusions
Candida spp. multiple-site colonization is frequently met among the critically ill medical patients. Broad-spectrum antibiotic therapy was found to promote fungal growth in patients with prior colonization. Since most of the invasive candidiasis in the ICU setting are thought to be subsequent to colonization in high-risk patients, reducing antibiotic use could be useful in preventing fungal infections.
Similar content being viewed by others
Introduction
Infections caused by Candida spp. among intensive care unit (ICU) patients are of growing interest. Invasive candidiasis diagnosis remains a challenge because rapidly available microbiological markers are not available. Most therapies are thereby initiated empirically in high-risk patients. Prior colonization could allow recognition of these patients [1, 2, 3]. Moreover, the risk of candidemia may be related to the density and to the extension of fungal colonization over time [3, 4]. Finally, since the risk of death was found to be similar in patients with multiple-site fungal colonization and those with confirmed invasive candidiasis, fungal colonization screening and management is a matter of concern [5].
Pittet and coworkers [3] proposed a clinically relevant colonization index in an attempt to assess fungal colonization density with time in high-risk surgical ICU patients. According to their results, the colonization index surveillance made possible the early recognition of patients in whom invasive candidiasis became manifest thereafter. Such patients were considered to be candidates for as the so-called preemptive antifungal therapy. Candida spp. colonization assessment based on multiple body site screening is now performed routinely in many ICUs [6, 7, 8]. Moreover, systemic treatments are considered as soon as the colonization index reaches the 0.50 threshold [9]. Such practices may lead to the overuse of antifungal and in turn to the risk of selection of resistant species [10, 11]. Since the question has not yet addressed, an assessment of such practices is needed [12, 13, 14, 15].
The colonization index has been evaluated among critically ill surgical patients. However, we have previously reported that the prior colonization density can be greater among critically ill medical patients with candidemia than in their surgical counterparts [16]. These findings raised the question of the assessment of the colonization index among critically ill medical patients. A prospective study was conducted in our medical intensive care unit (MICU) to assess the significance of the colonization index in this setting.
Patients and methods
Patients
All patients admitted to our eight-bed MICU between 1 August 2001 and 31 December 2002 were eligible provided their life expectancy exceeded 7 days. Exclusion criteria were: previous hospitalization in an ICU for more than 7 days within the past 30 days, length of stay less than 7 days, history of systemic fungal infection, neutropenia, antifungal therapy within the 7 days preceding ICU admission, and blood culture positive for Candida spp. at admission.
The main clinical and epidemiological data at ICU admission such as age, gender, admission severity of illness expressed by the Simplified Acute Physiology Score II (SAPS II), and severity of comorbidities expressed in terms of the score of McCabe and Jackson [17]. The length of stay in hospital prior to ICU admission was taken into account if it exceeded 3 days. Other variables included patient’s medical treatments thought to influence fungal colonization, medical devices, surgical procedures, and microbiological findings. Follow-up continued until patient death or discharge from the ICU.
Fungal surveillance cultures
Fungal surveillance cultures of the nose, throat, stool or rectal swab, urine, skin, and protected tracheal aspirates were taken at admission and then weekly until death or ICU discharge. Specimens were inoculated onto Sabouraud agar. Cultures were considered positive if at least 10 colony-forming units per milliliter (cfu/ml) were recovered after 48 h of incubation at 25°C. Yeast identification was based on a combination of microscopic examination and biochemical pattern study using the API 32C System (Biomérieux, Lyon, France). The Candida spp. colonization index was then calculated by the ratio of the number of culture-positive surveillance sites to the number of sites cultured. Blood samples were obtained by blood puncture at patient admission and then each time that two or more systemic inflammatory response syndrome criteria were present [18]. Blood samples were processed using the BACTEC system based on Mycosis* media coupled with the 9240 automate (Beckton Dickinson Diagnostic Instrument System, Paramus, N.J., USA).
Definitions
Fungal colonization was defined as a colonization index exceeding 0.20 (e.g., at least two samples of seven growing Candida spp.) [3]. Two consecutively obtained colonization index values reaching the 0.50 threshold were needed for the diagnosis of heavy colonization. Invasive candidiasis was considered confirmed if histopathological examination revealed typical patterns in a relevant clinical context [19]. Candidemia was defined as the isolation of Candida spp. in at least one blood culture in a patient with temporally related clinical signs. The diagnostic of candiduria required the recovery of at least 100 cfu/ml of the same Candida species in two distinct urine samples obtained within 1 week. Isolated candiduria was not considered as a candidal infection.
Clinical endpoints
Firstly, we looked for factors associated with heavy fungal colonization in the ICU. Two approaches were used: (a) patients who reached the 0.50 threshold were compared to those who did not; (b) a dynamic approach was used in an attempt to identify factors capable of influencing variations of the colonization index with time. Secondly, patient outcome was assessed. Given the study design and the rarity of invasive candidiasis in our ICU when reliable diagnosis criteria were used (fewer than five episodes per year [16]), the predictive value of the colonization index was not evaluated.
Statistical analysis
All quantitative data are presented as mean ±SD unless otherwise stated. The χ2 or Fisher’s exact test was used to compare categorical variables. Student’s t test for unpaired data was used to compare continuous variables. The Mann-Whitney U, test and the Wilcoxon rank test were used to compare continuous variables when they were not normally distributed. Logistical regression was used to examine the independent contribution of factors that had been predictive of heavy fungal colonization acquisition in the univariate analysis. Candidate variables were manually entered into the model if the associated regression coefficient had a p value less than 0.05. The independent contribution of factors to colonization index time variations was evaluated using a generalized estimating equation (GEE) population-averaged model, a nonparametric approach. The GEE provides a nonparametric random effects model based on an algorithm which is an extension of the method of maximum likelihood used in the logistic case. Variables included in this analysis were required to have a plausible relationship with the colonization index variations as well as a p value less than 0.05. A stepwise approach was used to determine which of the studied factors or variables were the most strongly associated with the colonization index variations. The duration of exposure to antibiotic therapy and duration of exposure to systemic antifungal medication were entered into this model as time-dependent variables.
Patient survival was calculated from the date of the ICU admission until death or discharge from the ICU. Cox’ proportional hazards regression analysis was used to examine the independent contribution of factors that had been univariately predictive of outcome with a p value less than 0.05. Heavy colonization was also included in the model because of its potential clinical relevance. Kaplan-Meier analysis was undertaken to describe survival in the groups stratified by the presence or the absence of systemic antifungal therapy. Curves were compared by means of the log-rank test. A p of 0.05 or less was considered to indicate statistical significance. The Statview software was used (SAS Institute, Cary, N.C., USA) except for the GEE population-averaged analysis (Stata statistical package, College Station, Tex., USA).
Results
Patients characteristics
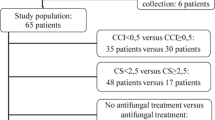
A total of 593 patients were admitted over the study period, 463 of whom were not included since their expected length of stay on admission was less than 7 days. Of the 130 patients originally included, 38 were subsequently excluded (neutropenia, n=1; ICU length stay less than 7 days, n=37). The study group thus included 92 patients (41 women, 51 men; mean age 66.7±15.5 years, range 21–92 years; Table 1). Twenty-eight (30.4%) had been hospitalized before ICU admission for a mean of 9.4±10.4 days (median 5, range 2–52).
The established risk factors for invasive candidiasis were present in most of the patients. Mean SAPS at admission was high (43.3±17.2), 83.7% required a mechanical ventilation for more than 3 days (mean 13.8±11.8, range 3–60), 83.7% had at least one central venous catheter for more than 2 days (mean 11.8±9.6, range 3–43), 73.9% had bladder catheterization for more than 2 days (mean 11.1±10.3, range 3–57), and 92.4% were exposed to broad-spectrum antibiotics for at least 2 days (mean 11.2±8.0, range 2–38). Systemic antifungal therapy (fluconazole, n=14; amphotericin B, n=8) was given to 22 patients for at least 2 days (mean 11.6±8.9). Twenty patients (90.9%) showed clinical symptoms of uncontrolled sepsis despite broad-spectrum antibiotic therapy as an antifungal agent was administered, and Candida spp. esophagitis was diagnosed in the remaining two. However, none of the patients received parenteral nutrition, and only eight (9.7%) underwent surgery during their ICU stay.
Fungal culture surveillance results
A total of 1,696 samples were taken over the study period for mycological examination. A mean of 18.4±10.4 samples per patient were obtained (median 16). Thus the mean number of available colonization index values for each patient was 3.2. Candida albicans was retrieved in 65.7% of the colonized patients, and C. glabrata in 10.9%. Other species were C. kefyr (6.8%), C. krusei (5.5%), C. parapsilosis (4.4%), and miscellaneous (7.2%). For each patient 7.7±7.4 blood samples were obtained for cultures, including 3.8±3.7 samples for cultures on Mycosis media. At ICU admission the mean colonization index was 0.26±0.26 (Table 2). No difference was found between previously hospitalized patients and the others (0.29 vs. 0.24, p=0.54). The colonization index increased significantly by 0.10 over the ICU stay (p=0.016; Fig. 1). Thirty-six patients (39.1%) reached the 0.50 threshold.
To determine which factor(s) predict such a degree of fungal colonization a logistical regression model, including variables univariately associated with the 0.50 threshold at p<0.05, was first performed (Table 3). Candida spp. colonization at ICU admission (odds ratio 18.8, 95% confidence interval, CI, 5.2–67.8, p<0.05) and bladder catherization for more than 2 days (OR=10.4; 95% CI 1.6–67.8, p<0.05) were found to be independently predictive of heavy colonization. There was no difference between the heavily colonized patients and others with regard to duration of hospital stay before admission to the ICU (9.5±8.0 vs. 9.4±12.2, p=0.75). Although heavily colonized patients were more likely to receive systemic antifungal therapy during their ICU stay (14, 61.1%, vs. 7, 12.5%), the difference was not found to be significant in our multivariate analysis model.
Secondly, the factor(s) influencing the colonization index were studied in a time-dependent fashion. The following factors were found to be independently associated with the increase in the colonization index: hematological malignancy (β=0.41, 95% CI 0.09–0.73, p<0.05), duration of exposure to broad-spectrum antibiotics (β=0.01, 95% CI 0.01–0.02, p<0.05), fungal colonization at ICU admission (β=0.19, 95% CI 0.11–0.28, p<0.05), and candiduria (β=0.20, 95% CI 0.10–0.30, p<0.05; Table 4). In contrast, the duration of exposure to antifungal agents was found to be significantly associated with a decrease in the colonization index (β=−0.02, 95% CI −0.03 to −0.01, p<0.05).
Patient outcome
The mean length of stay in the overall study population was 20.4±13.4 days (range 7–76 days; Table 1). However, it is worth noting that heavily colonized patients spent significantly more time in the ICU than the others (25.6±16.3 vs. 16.9±9.9 days, p=0.0015). The ICU crude mortality rate was 45.6% in the overall study population. The survival analysis was performed using a Cox model (Table 5). It was found that a rapidly fatal McCabe score (hazard ratio, HR, 4.33, 95% CI 1.29–14.70, p<0.05), duration of mechanical ventilation (HR 1.04, 95% CI 1.01–1.08, p<0.05), and duration of exposure to antibiotics (HR 1.06, 95% CI 1.01–1.10, p<0.05) were the only variables independently associated with a poor outcome. However, the probability of survival was comparable in the two groups (46.7% vs. 31.9%, respectively; HR 1.04, 95% CI 0.53–2.03, p=0.90). Only one patient met the criteria for the diagnosis of invasive candidiasis as defined above (positive skin biopsy specimen in a patient with septic shock and typical maculopapular rash). The last colonization index value available before fungal infection diagnosis was 0.57. It is noteworthy that no case of confirmed invasive candidiasis was reported over the study period among the patients who were not enrolled.
Discussion
The diagnosis of systemic candidiasis in critically ill patients requires surrogate markers. The colonization index has been reported as a convincing diagnostic tool to detect high-risk patients for whom a preemptive therapy could improve the outcome [3], with the 0.50 threshold differentiating between high-risk patients and others (sensitivity=100%, specificity=66.7%) provided other invasive candidiasis risk factors including surgical procedures are present.
We present several findings regarding the colonization index in an MICU population. A large proportion of our patients (45.6%) were already colonized at the time of admission to the ICU, as reported in surgical patients [20, 21, 22]. Interestingly, the mean colonization index value at ICU admission in the study population (0.26) was similar to that recently reported in postoperative patients [23]. Medical critically ill patients may therefore exhibit fungal colonization levels near from those observed in their surgical counterparts [16]. However, the inclusion protocol may have precluded our results validity since many patients were not included because their length of stay expectancy was too short. We introduced thus a recruitment bias that might exclude the most severely ill patients whose predicted survival was short, as well as those with a short stay in the ICU because of a rapidly good outcome. In addition, the study population was not strictly medical since eight patients underwent surgical procedure during their ICU stay. However, surgery was never abdominal and diagnosis on admission was always medical. Finally, these patients did not differ from the others in terms of age, gender, SAPS II, outcome, ornd colonization index values.
Both static and dynamic approaches of the fungal colonization were used in the present study since the risk of invasive candidiasis seemed to be related both to its density at a given time and to its extension with time [3, 4]. We found that the presence of fungal colonization on ICU admission was independently associated with a subsequent colonization index superior or equal to the 0.50 threshold. It is worth noting that such patients with prior colonization were not found to differ from those without, especially with regard to baseline severity of illness and duration of hospital stay within the 30 days preceding their ICU admission. Since this factor could not be reliably assessed, one cannot exclude the possibility that colonized patients were more likely to have received broad-spectrum antibiotics prior to ICU admission. Indeed, a previous study found that bacterial infection in the month preceding ICU admission was the only risk factor associated with fungal colonization [22]. The shortness of the length of stay prior to ICU admission (2.9±7.1 days) made such conclusion unlikely. Furthermore, antibiotics may have been administered at home to these patients. In any case, this finding suggests that in the present study Candida spp. colonization developed from the already colonized patients’ own flora whereas newly acquired fungal colonization was unlikely. Such a conclusion should of course be taken cautiously since no genotyping method was used.
As expected, bladder catherization was independently associated with heavy colonization [7, 24, 25]. Since candiduria was present in most of the patients who exhibited a high colonization index, this finding suggest that the Foley catheter favored urine colonization with Candida spp. as previously found [7, 25].
Our dynamic approach showed that the duration of antibiotic treatment was independently associated with a growing colonization index. It has been known for long time that broad-spectrum antibiotics could lead to yeast overgrowth within the gut flora [26, 27]. Moreover, such an association between antibiotic consumption and the variation in fungal colonization index has already been noted in surgical patients [8]. However, it could be a marker of disease severity rather than a direct contributive factor. Accordingly, our multivariate analysis did not identify the antibiotic therapy length as an independent predictor for heavy fungal colonization.
The duration of a systemic antifungal treatment was associated with a decrease in the colonization index in a time dependent manner according to the GEE analysis [23, 28]. However, any conclusion regarding this point remains elusive since only a few selected patients (i.e., the most colonized ones) received such a treatment. In addition, our logistic regression analysis model failed to confirm this result.
We were unable to establish the reported relationship between the risk of confirmed invasive candidiasis and the colonization index value, since only one episode occurred during the study period [3]. Furthermore, the colonization index was not determined daily as it was in the original study, and no molecular typing was carried out to ensure that yeasts from the same species that colonized one patient belonged to a single strain [29]. Therefore one cannot exclude that our colonization index overvalued fungal colonization as compared to that of Pittet et al. [29]. This could in turn lead to a lower specificity. However, our study was designed in an attempt to evaluate a fungal colonization density follow-up which could be applied routinely in an ICU setting, given the work load excess generated by multiple-sites fungal screening.
Finally, although there was a trend toward greater mortaliy in the ICU among the heavily colonized patients than in the others (46.7% vs. 31.9%, p=0.90), the risk of death was not related to fungal colonization density as previously reported [5, 30]. However, the small size of the sample may account for our failure to demonstrate any statistically significant difference. Nevertheless, heavily colonized patients seemed to be more critically ill than the others since both ICU length of stay and the incidence of ventilator-associated pneumonia was greater in this group (data not shown).
In conclusion, colonization with Candida spp. was common in our MICU population. Such patients could be identified upon ICU admission since high colonization index values (e.g., superior or equal to the 0.50 threshold) were found almost exclusively in patients with elevated baseline values. Broad-spectrum antibiotic therapy was found to be the main factor likely to enhance independently fungal colonization in a time dependent manner. Our analysis failed, however, to identify any difference in outcome related to the colonization index. Moreover, the predictive value of the colonization index regarding the risk of invasive candidiasis could not be established. Our findings suggest that limiting the use of broad-spectrum antibiotics in the ICU could prevent Candida spp. colonization and in turn potentially reduce the risk of subsequent invasive candidiasis [31].
References
Bross J, Talbot G, Maislin G, Hurwitz S, Strom B (1989) Risk factors for nosocomial candidemia: a case-control study in adults without leukemia. Am J Med 87:614–620
Wey S, Mori M, Pfaller M, Woolson R, Wenzel R (1989) Risk factors for hospital-acquired candidemia. Arch Intern Med 149:2349–2353
Pittet D, Monod M, Suter P, Frenk E, Auckenthaler R (1994) Candida colonization and subsequent infections in critically ill surgical patients. Ann Surg 220:751–758
Calandra T, Bille J, Schneider R, Mosimann F, Francioli P (1989) Clinical significance of Candida isolated from peritoneum in surgical patients. Lancet II:1437–1440
Slotman G, Shapiro E, Moffa S (1994) Fungal sepsis: multisite colonization versus fungemia. Am Surg 60:107–113
Tran L, Auger P, Marchand R, Carrier M, Pelletier C (1997) Epidemiological study of Candida spp. colonization in cardiovascular surgical patients. Mycoses 40:169–173
Dubeau B, Triboulet C, Winnock S (2001) Utilisation pratique de l’index de colonisation. Ann Fr Anesth Reanim 20:418–420
Yazdanparast K, Auger P, Marchand R, Carrier M, Cartier R (2001) Predictive value of Candida colonization index in 131 patients undergoing two different cardiovascular surgical procedures. J Cardiovasc Surg (Torino) 42:339–343
Munoz P, Almudena B, Bouza E (2000) Criteria used when initiating antifungal therapy against Candida spp. in the intensive care unit. Int J Antimicrob Agents 15:83–90
Gleason T, May A, Carapelli D, Farr B, Sawyer R (1997) Emerging evidence of selection of fluconazole-tolerant fungi in surgical intensive care units. Arch Surg 132:1197–1202
Safran D, Dawson E (1997) The effect of empiric and prophylactic treatment with fluconazole on yeast isolates in a surgical trauma intensive care unit. Arch Surg 132:1184–1189
British Society for Antimicrobial Chemotherapy Working Party (1994) Management of deep Candida infection in surgical and intensive care unit patients. Intensive Care Med 20:522–528
Edwards JJ, Bodey G, Bowden R, Buchner T, de Pauw B, Filler S, Ghannoum M, Glauser M, Herbrecht R, Kauffman C, Kohno S, Martino P, Meunier F, Mori T, Pfaller M, Rex J, Rogers T, Rubin R, Solomkin J, Viscoli C, Walsh T, White M (1997) International Conference for the Development of a Consensus on the Management and Prevention of Severe Candidal Infections. Clin Infect Dis 25:43–59
Rex J, Walsh T, Sobel J, Filler S, Pappas P, Dismukes W, Edwards J (2000) Practice guidelines for the treatment of candidiasis. Clin Infect Dis 30:662–678
Pappas P, Rex J, Sobel J, Filler S, Dismukes W, Walsh T, Edwards J (2004) Guidelines for treatment of candidiasis. Clin Infect Dis 38:161–189
Charles PE, Doise JM, Quenot J, Aube H, Dalle F, Chavanet P, Milesi N, Aho L, Portier H, Blettery B (2003) Candidemia in critically ill patients: difference of outcome between medical and surgical patients. Intensive Care Med 29:2162–2169
McCabe W, Jackson G (1962) Gram-negative bacteremia. Arch Intern Med 110:847–855
Bone R (1993) The pathogenesis of sepsis. Ann Intern Med 115:457–469
Ascioglu S, Rex J, DePauw B, Bennett J, Bille J, Crokaert F, Denning D, Donnelly J, Edwards J, Erjavec Z, Fiere D, Lortholary O, Maertens J, Meis J, Patterson T, Ritter J, Selleslag D, Shah P, Stevens D, Walsh T (2002) Defining opportunistic invasive fungal infections in immunocompromized patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 34:7–14
Petri M, Konig J, Moecke H, Gramm H, Barkow H, Kujath P, Dennhart R, Schafer H, Meyer N, Kalmar P, Thulig P, Muller J, Lode H (1997) Epidemiology of invasive mycosis in ICU patients: a prospective multicenter study in 435 non-neutropenic patients. Paul-Ehrlich Society for Chemotherapy, Divisions of Mycology and Pneumonia Research. Intensive Care Med 23:317–325
Vincent JL, Bihari D, Suter P, Bruining H, White J, Nicolas-Chanoin M, Wolff M, Spencer R, Hemmer M (1995) The prevalence of nosocomial infection in intensive care units in Europe. Results of the European Prevalence of Infection in Intensive Care (EPIC) Study. EPIC International Advisory Committee. JAMA 274:639–644
Hedderwick SA, Lyons MJ, Liu M, Vazquez JA, Kauffman CA (2000) Epidemiology of yeast colonization in the intensive care unit. Eur J Clin Microbiol Infect Dis 19:663–670
Garbino J, Lew DP, Romand JA, Hugonnet S, Auckenthaler R, Pittet D (2002) Prevention of severe Candida infections in nonneutropenic, high-risk, critically ill patients: a randomized, double-blind, placebo-controlled trial in patients treated by selective digestive decontamination. Intensive Care Med 28:1708–1717
Vincent JL, Anaissie E, Bruining H, Demajo W, el-Ebiary M, Haber J, Hiramatsu Y, Nitenberg G, Nystrom P, Pittet D, Rogers T, Sandven P, Sganga G, Schaller M, Solomkin J (1998) Epidemiology, diagnosis and treatment of systemic Candida infection in surgical patients under intensive care. Intensive Care Med 24:206–216
Kauffman C, Vazquez J, Sobel J, Gallis H, McKinsey D, Karchmer A, Sugar A, Sharkey P, Wise G, Mangi R, Mosher A, Lee J, Dismukes W (2000) Prospective multicenter surveillance study of funguria in hospitalized patients. Clin Infect Dis 30:14–18
Samonis G, Gikas A, Toloudis P, Maraki S, Vrentzos G, Tselentis Y, Bodey G (1994) Prospective study of the impact of broad-spectrum antibiotic on the yeast flora of the human gut. Eur J Clin Microbiol Infect Dis 13:665–667
Stone H, Kolb L, Currie C, Geheber C, Cuzzell J (1974) Candida sepsis: pathogenesis and principles of treatment. Ann Surg 179:697–710
Laverdière M, Rotstein C, Bow E, Roberts R, Ioannou S, Carr D, Moghaddam N, Group CFS (2000) Impact of fluconazole prophylaxis on fungal colonization and infection rates in neutropenic patients. J Antimicrob Chemother 46:1001–1008
Pittet D, Monod M, Filthuth I, Frenk E, Suter PM, Auckenthaler R (1991) Contour-calpmed homogenous electric field gel electrophoresis as a powerful epidemiologic tool in yeast infections. Am J Med 91 [Suppl 3B]:256S–263S
Ibanez-Nolla J, Nolla-Salas M, Leon MA, Garcia F, Marrugat J, Soria G, Diaz RM, Torres-Rodrigues JM (2004) Early diagnosis of candidiasis in non-neutropenic critically ill patients. J Infect 48:181–192
Sandven P, Bevanger L, Digranes A, Gaustad P, Haukland H, Steinback M, Group TNYS (1998) The constant low rate of fungemia in Norway, 1991 to 1996. J Clin Microbiol 36:3455–3459
Acknowledgements
This research was presented at the Congress of the French Society of Critical Care Medicine, January 2004.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Charles, P.E., Dalle, F., Aube, H. et al. Candida spp. colonization significance in critically ill medical patients: a prospective study. Intensive Care Med 31, 393–400 (2005). https://doi.org/10.1007/s00134-005-2571-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2571-y